
Doctors working to limit the spread of syphilis, chlamydia and gonorrhea — and their potential complications if left untreated — are turning to a promising new means of prevention.
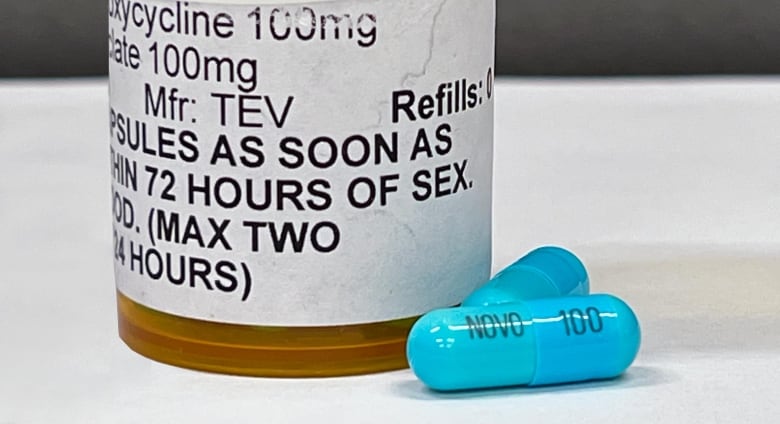
It’s known as DoxyPEP, which stands for doxycycline (an antibiotic) post-exposure prophylaxis.
Some liken it to a “morning-after pill,” as you take it after sexual activity that may have left you at risk of contracting an STI.
For Dustin Hutton-Alcorn, a 33-year-old gay man in Abbotsford, B.C., having DoxyPEP on hand offers him some peace of mind that he has an additional means of protecting his sexual health.
“[It] allows me to be a responsible adult, especially in the queer community,” he told CBC News.
The efficacy of DoxyPEP was studied in people at elevated risk for STIs: two-spirit, gay, bisexual, and queer cisgender men and transgender women. The small but growing number of studies showed it significantly reduced the risk of contracting syphilis, chlamydia and — to a lesser extent — gonorrhea among those groups.
But access to DoxyPEP is limited, depending on where you live, and it’s not a federally approved treatment, which may create further barriers to availability and awareness.
The Current15:57Tackling rising syphilis cases across Canada
Syphilis infections are surging across Canada, including cases of babies born with congenital syphilis. We talk to Dr. Darrell Tan, an infectious disease specialist at St. Michael’s Hospital in Toronto; and Caroline Cameron, a professor in the department of biochemistry and microbiology at the University of Victoria in B.C.
DoxyPEP not for everyone, not a silver bullet
Doxycycline is a commonly used antibiotic that health-care providers may prescribe to treat some bacterial infections — including syphilis and chlamydia — as well as conditions like acne and rosacea and to prevent malaria. It has minimal potential side effects, including stomach upset and sensitivity to sun.
DoxyPEP is similar to a method of HIV prevention known as PrEP (pre-exposure prophylaxis) that sees 2SGBTQ+ people at risk of contracting HIV take a daily dose of an anti-retroviral medication.

PrEP has proven to be highly effective in reducing the risk of getting HIV from sexual activity, when taken as prescribed, virtually eliminating the risk of contracting the virus that causes AIDS.
DoxyPEP’s 200-milligram dose is best taken within 24 hours, but no later than 72 hours after condomless oral or anal sex.
There is compelling evidence that it’s effective in preventing sexually transmitted bacterial infections, said Dr. Peter Phillips, an infectious diseases specialist and member of the DoxyPEP program at the B.C. Centre for Excellence in HIV/AIDS (BC-CfE).
Three randomized controlled studies have shown that doxycycline taken post-exposure can reduce the risk of being infected with syphilis and chlamydia by more than 70 per cent, Phillips said. That includes one conducted in California, the first jurisdiction in North America to implement guidelines on DoxyPEP.
It was less successful in preventing gonorrhea infections, but still reduced the risk by about 50 per cent, he said.
There isn’t conclusive evidence, however, that DoxyPEP is of any benefit to cisgender women, people assigned female at birth or transgender men, he said, pointing to a study conducted in Kenya that did not show any benefit for cis women.
Most at risk eligible for DoxyPEP
Although the number cases and infection rates for syphilis are lower compared to those for chlamydia and gonorrhea, the infection can lead to severe complications, possibly affecting organ function, if it’s not treated early on, Phillips said.
Other prevention approaches — such as condoms, sexual education, testing and contact tracing — have not been enough to slow the spread of syphilis, he said.
The BC-CfE began offering DoxyPEP to eligible patients, free of charge, with the support of the B.C. government in December — the first such program in Canada.
To meet the criteria, an individual must be enrolled in the BC-CfE’s PrEP program for HIV prevention or be someone who is HIV-positive and taking anti-retroviral therapy drugs to both remain healthy and reduce the risk of transmission.
They must also have contracted chlamydia, gonorrhea and/or syphilis in the past year, or have been clinically assessed as being at increased risk.
There are already 2,300 people signed up for the BC-CfE’s DoxyPEP program, Phillips said, and that number increases by about 300 each month.
Phillips said it’s too early to provide any conclusive findings on the success of the program, as it’s been less than a year since it launched. But he said there’s no reason B.C. wouldn’t see the same success that California and other jurisdictions have.
A University of Victoria microbiologist is leading a team of researchers to develop a vaccine for syphilis, after health officials say cases are rising once again in North America. CBC’s Climate and Science Specialist Darius Mahdavi spoke to Caroline Cameron to find out why a syphilis vaccine is needed.
Canadian research underway
PHAC confirmed to CBC News that it is reviewing published evidence to “support the development of recommendations” for DoxyPEP, but did not indicate a timeline.
The U.S. Centers for Disease Control and Prevention released finalized clinical guidance on DoxyPEP in June.
But the existing data on DoxyPEP is enough to outweigh any hesitancy about prescribing it, according to Drew Schnobe, a pharmacist and team lead at The PrEP Clinic, a private online service launched in Ontario in 2019 to provide better access to HIV PrEP and now DoxyPEP.
“We don’t want to withhold something that people could benefit from when we do have information and when we do have real-world experience with these already,” he said.
Health Canada has also not approved doxycycline as a preventive treatment for STIs, but the department told CBC News it has not received any submissions to specifically review DoxyPEP.
That’s unlikely to happen, due to doxycycline being a generic medication that is already approved for widespread use, said Dr. Caley Shukalek, an internal medicine physician.
“No one’s going to pay the fee to apply to get that labelling.”
As a result, DoxyPEP is prescribed off-label — when a drug is used for conditions other than what it was originally approved to treat.
“Many drugs are used off-label because there’s clinical evidence to do so,” said Shukalek, who is the chief medical officer at Calgary-based PurposeMed, which operates Freddie, another private virtual provider of prescriptions for both HIV PrEP and DoxyPEP.
And there are efforts to add to that body of research, he said.
Shukalek is a member of a Canadian research team conducting an open-label randomized controlled study of 560 participants, in multiple locations, known as the Doxycycline as an Intervention for bacterial STI ChemOprophylaxis — or DISCO for short.
Participants will be randomly assigned to take either DoxyPEP or DoxyPReP.
DoxyPrEP is a daily dose of doxycycline as opposed to only taking a dose after a sexual encounter. It is not currently offered as an STI treatment.
Yukon Morning7:30An infectious disease specialist on the rise of syphilis
Syphilis is on the rise in Canada. In the Yukon, there have been 117 infections since 2022. Dr. Ameeta Singh studies infectious diseases at the University of Alberta. She has served as the Territorial Consultant for Sexually Transmitted and Blood Borne Infections in Nunavut since July 2017.
Limited access
Despite evidence supporting its use, health-care providers and sexual health clinics in some places may not offer DoxyPEP until there is federal approval or guidance, warned Chris Aucoin, the executive director of Health Equity Alliance of Nova Scotia (HEAL NS), formerly known as the AIDS Coalition.
“There’s definitely no infrastructure … to say, ‘Here’s what it is,'” he said of the situation in that province, noting that access to HIV PrEP is limited and STI testing isn’t widely available outside Halifax.
Someone may be able to approach their doctor, he said, but virtual services like Freddie and the PrEP Clinic aren’t an option.
The PrEP Clinic only operates in Ontario. Freddie only offers its services in British Columbia, Alberta, Saskatchewan, Manitoba and Ontario — jurisdictional hurdles prevent it from expanding into some places like Nova Scotia, Shukalek explained.
Even people in places with easier access may have difficulty finding out about DoxyPEP, said Hutton-Alcorn.

He switched to using Freddie for his HIV PrEP about a year ago, rather than continuing with the BC-CfE program, as it became too arduous to sort out regular STI testing and prescription delivery, living 70 kilometres away from downtown Vancouver.
He said he likely wouldn’t have known he had access to DoxyPEP if it hadn’t been for a prompt when he was renewing his HIV PrEP prescription around six months ago.
“But it’s not just about giving access to the medication. It’s about giving access to health-care resources and education,” he said.
“And contrary to popular belief, there are queer people that live outside of downtown Vancouver.”
Richard MacDonagh and J.P. Chua with London Intercommunity Health Centre joined London Morning to talk about the importance of getting tested for HIV and their disappointment that the federal government is no longer funding a self-testing kit program.

