
When Patricia Keesickquayash looks atop the hill of her First Nation’s cemetery, which was expanded in the 1990s, she wonders how the plots filled up so quickly.
Unnatural death rates in First Nations across the Sioux Lookout area of northwestern Ontario are more than triple the provincial average.
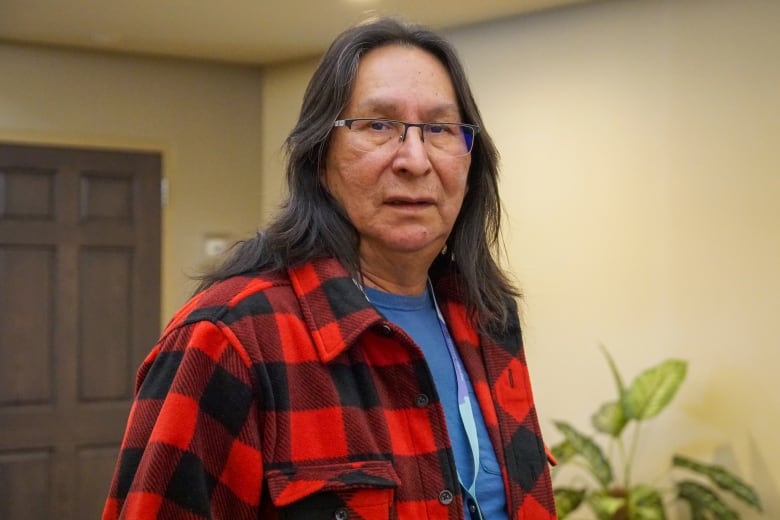
“This is reality for us,” said Keesickquayash, health director of Mishkeegogamang Ojibway First Nation, about 500 kilometres northwest of Thunder Bay.
The Sioux Lookout First Nations Health Authority (SLFNHA) provides services for 33 First Nations, most of which are remote. Its “Mental Health and Substance Use” report, which was released this week, includes data from 2011 to 2021 on how its communities are disproportionately affected by mental illness and addictions.
The report begins with first-person accounts, including Keesickquayash’s story. It’s the first time she’s spoken publicly about her experiences with addiction and trauma.
“Throughout my childhood … it was shushed. We couldn’t talk about it and nobody would listen.”
Over the past year, First Nations leaders have been ramping up advocacy efforts for better health care:
SLFNHA and area leaders are calling on the provincial and federal governments to support First Nations in delivering better mental health and addiction services within their communities.
“The communities know exactly what they want to do and how they want to address the issue. Resources are therefore required — resources that are sustainable, long-term funding to address the issues,” said Dr. Lloyd Douglas, public health physician with SLFNHA.
“We need to see more workers at the community level and all the agencies working together in a way so that the vision of this model can be achieved.”
‘I’ll start the healing cycle with our family’
Keesickquayash was eight years old the first time she got high on solvents. She experienced physical and sexual abuse during her childhood, and domestic abuse in her early adulthood. She leaned on alcohol to cope.
But once she learned about the legacy of residential schools — her father was forced to attend — she came to understand the trauma that has inflicted tragedy across generations of her family, she explained.
“As a part of my honour to my father … I’ll start the healing cycle with our family,” she said.
Now well into her healing journey, Keesickquayash hopes her story inspires others to share their experiences, and that these stories can make a difference in First Nations.

Mental health and substance use was the fourth most common reason for nursing station visits across SLFNHA communities between 2015 and 2021, according to SLFNHA’s report.
In 2021:
- Emergency department visit rates for intentional self-harm and injury were 16 times higher than the provincial rate.
- Emergency department visit rates for mental health and substance use were 14 times higher than the provincial rate.
- Hospitalizations for mental health and substance use were more than six times higher than the provincial rate.
“We have struggled to get adequate information about the communities that we work with,” said Janet Gordon, SLFNHA’s chief operating officer. “This just confirms that the picture is way worse than what we hear on a daily basis.”
Federal government responds to report
CBC News reached out to the office of Minister of Indigenous Services Patty Hajdu and received an emailed statement from her press secretary.
“The SLFNHA is doing crucial work for communities, and we will always be there to support their efforts,” wrote Jennifer Kozelj. “We are also supporting access to mental wellness services for First Nations across Northern Ontario. Through NAN Choose Life, over half a billion dollars will support First Nations-led initiatives on mental wellness, so every child has a fair chance to succeed.”
Kozelj said Hajdu recently visited Mishkeegogamang and heard directly from community members about how they support youth.
“There is still more work to do so First Nations youth have the same level of services as other Canadians, and we want to hear from partners on how we can improve our ways of working to achieve this goal.”
“Ultimately, First Nations know what they need best, which is why we want to support a more self-determinate approach,” said Kozelj. “We are more than open to start discussions on stable long-term funding. We will follow First Nations’ lead and will support their priorities the way they want us to.”
Earlier this year, Ontario announced $2.6 million to support mental health and addictions services delivered by NAN.
Benefits of land-based treatment
Cat Lake First Nation Chief Russell Wesley lost his wife to medical-related addiction issues. Since his election as chief in 2020, he said, there have been 37 unnatural deaths in his community.
He said that since the release of the SLFNHA report, there have been three overdoses and five suicides in Cat Lake, which is about 440 kilometres northwest of Thunder Bay along the Albany River.
More than a decade ago, a crisis of solvent abuse in the community was treated with land-based programming, which Wesley said is no longer in place.
“The land-based components reconnect individuals back to their spirituality and their personal relationship with their Creator,” he said. “The clinical treatment doesn’t have that component.”
Wesley is seeking funding and policy directives to support the return of land-based treatment. For now, a treatment centre is anticipated to be ready by August or September and a language program is planned for the fall.
Regionally, SLFNHA is marking a win through a new partnership with Eagle Lake First Nation and the Kenora District Services Board to build a regional healing lodge in the First Nation.
The healing lodge will provide mental health support services to SLFNHA communities, which include Cat Lake, with a focus on drug and alcohol treatment.
Training community members
Keesickquayash said she has already been approached by several people commending her for sharing her lived experience of addiction.
To her, solutions must be driven by community members; she’s seen too many people give up on counselling after struggling to maintain rapport with workers who come in and out of the First Nation.
“If we were to train our front-line workers about community addictions, about grief counselling and trauma counselling … we’d have more permanent people in the community that [patients] have built relationships with,” Keesickquayash said.
Mishkeegogamang has a nursing station and offers NAN’s Choose Life program, but she also wants to see a treatment centre, a detox centre, and a space where people can share their experiences without judgment.
When it comes to healing from trauma, “they say it takes seven generations,” said Keesickquayash. “I’m starting with me and my family.”
If you or someone you know is struggling, here’s where to get help:
Kenora & Northwestern Ontario Resources:
- Kenora Makwa Patrol Help Line: (807) 464-SAFE (7233) Open 24/7. Support program that helps connect vulnerable populations to services in Kenora.
- Kenora Chiefs Advisory Crisis Services: (807) 468-8144, ask for intake. Available 9 a.m. to 5 p.m. CT for people in Kenora and surrounding First Nations.
- Thunder Bay Crisis Response: (807) 346-8282 Open 24/7 to anyone from Kenora east to Wawa. Access trained crisis response workers by calling, texting or chatting online via the CMHA website.
- Nishnawbe Aski Mental Health and Addictions Support Access Program 1-844-NAN-HOPE (626-4673) Open 24/7. Crisis support phone line for NAN members.
Canada-Wide Resources:
- Suicide Crisis Helpline: Text or call 9-8-8 for mental health support. Open 24/7.
- Hope for Wellness: 1-855-242-3310 Open 24/7. Provides free phone and live online chat counselling on the website for Indigenous people. Support available in Ojibway (Anishinaabemowin), Cree and Inuktitut upon request.
- Kids Help Phone: 1-800-668-6868. Open 24/7. Free phone and live chat counselling on the website for youth in Canada.
- Canadian Association for Suicide Prevention: Find a 24-hour crisis centre.
This guide from the Centre for Addiction and Mental Health outlines how to talk about suicide with someone you’re worried about.