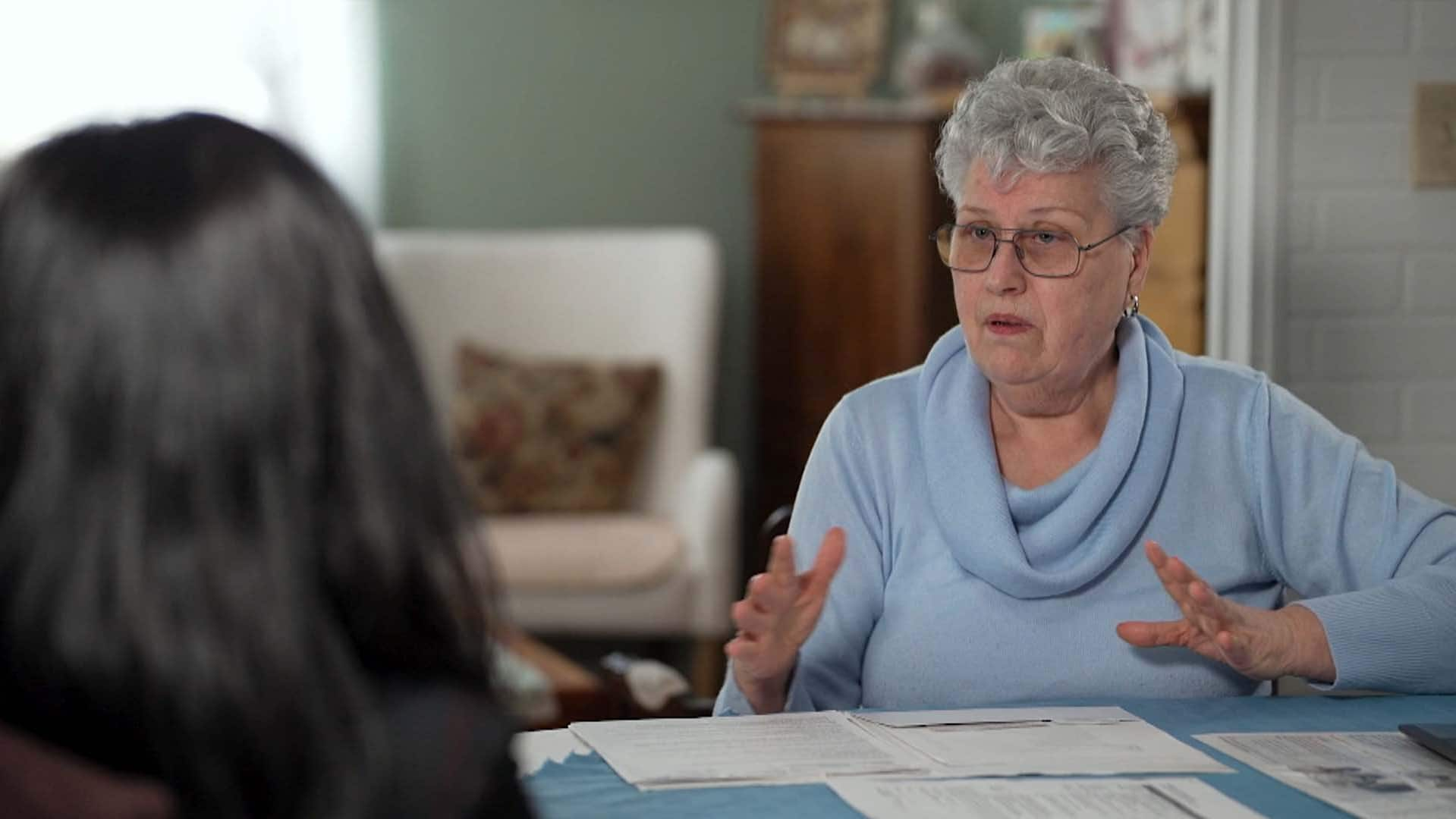
Lois Cooper says she was upsold thousands of dollars in extra services at a private, for-profit clinic, and when she started to ask questions, the doctor told her to leave. She’s not the only Canadian who’s gone through the questionable practice.
It’s the pile of bills that sums up her medical journey.
“This is the note that I made when I got the phone call in January,” said the 75-year-old from Gravenhurst, Ont. “And I was told there’d be a $150 fee…. That was the beginning of starting to pay for stuff.”
Cooper had a macular hole in her right eye and needed medically necessary surgery called a vitrectomy, a procedure where the surgeon removes the gel-like substance around the eye called the vitreous and replaces it with another solution.
Cooper was referred to a private, for-profit clinic north of Toronto, but before the operation started, she was asked to sign off on optional tests, services and procedures.
In later appointments following the surgery, the doctor told her that she would need to keep her face down for two weeks — and that would require the rental of a special wedge type of pillow. He also recommended glasses that would refract her vision. Months later, he recommended laser surgery for eye floaters, which Cooper said didn’t work. He even said he detected a mass behind her other eye that would require further surgery.
A second opinion from a doctor in Toronto revealed there was no mass in her eye.
Health Canada reports show private, for-profit clinics are upselling patients on extra services they don’t need. One Ontario patient says a private clinic had her sign off on additional services that cost her thousands and even tried to get her to have another surgery that she didn’t need.
When Cooper asked questions, she was shown the door — but not before she was on the hook for close to $8,000 for appointments, equipment rentals and procedures.
Cooper was upsold.
“I wouldn’t have spoken out if I hadn’t heard Premier [Doug] Ford say that these private clinics won’t charge you money, won’t charge extra,” she told CBC News. “It feels like it’s my public duty to say that’s not true.”
What is upselling?
Upselling, according to Dr. Danyaal Raza, a family doctor at St. Michael’s Hospital in Toronto, occurs when a patient is asked to pay for extra services that are uninsured when they’re undergoing a procedure that should be publicly covered.
It’s different from extra billing. That’s when a private, for-profit clinic would bill the province for a procedure that’s covered by government health insurance while also billing the patient.
Health Canada reports show that between April 2019 and March 2020, private, for-profit clinics upsold and illegally charged Canadians to the tune of tens of millions of dollars.

In early March, the federal government announced that it was going to cut more than $82 million in transfer payments to the provinces in cases where patients were asked to pay out of pocket for care that should have been covered in 2020-21.
“You’re paying out of pocket for health care you should not be paying for and clinics are prohibited from charging you,” said Andrew Longhurst, a health policy researcher at Simon Fraser University in Vancouver.
Raza said it’s a slippery slope between extra billing and upselling.
“I think we need to be concerned about upselling because it’s the thin edge of the wedge towards extra billing, where patients are told they can only get something that’s publicly covered if they pay out of pocket.”
How does upselling work?
Upselling can start with the power dynamic that often exists between patients and health-care professionals. Cooper said it certainly started that way for her.
“I was sent there by my medical professional. So that would mean to me that this is where you should be and this is how it’s done, and this is what’s expected and you do it.”
Once she got to what she described as a “large warehouse with no ceiling” that was packed with people, she had to sign documents before she was seen by anyone.
With a recent poll showing Canadians are divided over privatizing health care, CBC’s Christine Birak looks into common questions about it, including patient outcomes and its impact on the public health care system.
It’s a situation, according to Raza, that’s filled with subtle pressure.
“You’re not a doctor, you’re not a nurse. You don’t have 10 years of medical training under your belt. So you’re at a huge disadvantage when you’re presented with information,” he said.
Cooper signed the documents, which she showed to CBC News, and had her vitrectomy. During the surgery, she said, her retina was torn and she was told cataracts were removed, even though Cooper had never been aware that she had cataracts.
She said she got her vision back in her right eye. However, in subsequent visits that cost her $150 for each appointment, the surgeon said he found a cataract in her other eye, told her she had dry eye disease and convinced Cooper to get laser surgery for floaters.
What’s more, that equipment Cooper’s doctor told her to rent after the initial surgery, such as the special glasses and pillow, should have been covered by the government since it was deemed to be a medically necessary procedure.
The bills have eroded Cooper’s trust in a medical system that should be protecting patients.
“I don’t know if it’s illegal, but it’s unethical. I think that the behaviour is unethical,” she said.
Cooper did not want to publicly name the clinic. CBC News reached out to the clinic for comment but did not receive a response.
In the face of a health-care crisis, Adrienne Arsenault brings together patients and health-care workers with different perspectives to discuss the problems, potential solutions and whether there’s a role for more privatization.
Why should we be concerned about upselling?
Dr. David Urbach, surgeon-in-chief at Women’s College Hospital in Toronto, said upselling is baked into the business model of public money going to private, for-profit clinics.
“I don’t believe they can be a viable business unless they’re going to be paid in excess of what the government is already paying public hospitals, or they’re going to be levying all these unnecessary charges,” he said.
What worries Raza is what he calls “the slow creep”: As more patients are persuaded to spend money on additional tests and procedures, they may grow accustomed to the practice.
“If you’re already used to paying for services that are uninsured out of pocket, suddenly paying for this insured service feels normal,” he said.
What can the public do?
Ultimately, Cooper started asking questions when she was told there was a mass in her eye that would require another vitrectomy.
“I asked him to explain the mass to me, and he looked at me like I had three heads,” she recalled.
When she asked further questions, the ophthalmologist told her to leave. “And then he turned to his assistant and said, ‘Charge this to OHIP.'”
In spite of her ordeal, Cooper is happy that the original surgery to fix the hole in her eye was successful. Her vision isn’t perfect, but she can read and drive. But her story is a cautionary tale, and she wants others to learn from it.
“I just want people to be aware that when they go to a private clinic, make sure you ask questions, don’t sign any papers. Go there first and get all the information on what they’re going to want from you and then maybe go talk to somebody else,” Cooper said.
“If you’re in a medical appointment and you’re being asked to pay for a medical service, you should always ask whether or not you need to pay that fee to actually get the care that you came there for,” Raza said.
He added that if a patient feels they were unfairly charged for a medical service performed at a hospital, they should contact the hospital’s patient relations department.
Unfortunately, Raza said, too much is put on the patient to process at a time when they are most vulnerable.
“If I ask, ‘Am I going to be denied care, am I going to be put at the back of the line?’ – it’s overwhelming, and frankly we shouldn’t really be expecting or asking patients to be able to decode federal and provincial legislation.”