
White Coat Black Art26:30The Real Good Doctor
Dr. JJ Mráček knew since she was a kid that she would one day go to medical school. But once she got there, the journey was rockier than expected.
Despite previous success in school — including a master’s degree in social work — Mráček struggled to find her footing in medicine.
Exams proved harder than expected. She felt ostracized by peers who, she says, saw her as “too loud” for a hospital. A strong sense of justice, and a need for structure, led to conflict with her supervisors who perceived her as too direct.
Then, just before she finished med school, Mráček got a diagnosis at age 32 that felt like a puzzle being finished: she is autistic.
“It felt like every uncertainty I’ve ever had about myself was answered in that moment — a lifetime of feeling just slightly out of place,” the Edmonton-based student told White Coat, Black Art host Dr. Brian Goldman.
“It really tied together every difficulty I’d ever experienced from a social perspective and gave me a singular answer, which we love in medicine. We love the unifying diagnosis.”
Mráček wants med schools and health-care institutions to work toward a culture that’s more accepting of doctors and trainees who are neurodiverse — a term describing differences in how people experience and interact with the world.
That could include, she says, better “flexibility” in accommodations for standard practices like the length of hospital shifts, some of which can be as long as 26 hours.
“In order to get into medical school, not only do you have to be intelligent, capable, empathetic, hard-working, but there’s this invisible presumption that you don’t have a disability,” Mráček said.
“This assumption we have — that we are all the same — I think that’s where that is rooted.”
Misconceptions about autism
Autism spectrum disorder (ASD) is a developmental condition that can impact a person’s communication and social skills, with varying severity from one person to the next.
There’s no consensus on the number of doctors formally diagnosed with ASD — in part because doctors may feel uncomfortable revealing a diagnosis for fear of discrimination, says Laura Carravallah, student and membership lead for Autistic Doctors International.
Autistic Doctors International, a research and advocacy organization for autistic medical doctors, has over 600 members.
There are common misconceptions among patients and colleagues about doctors with autism. For example, some people may respond to a common scenario differently from one day to the next, depending on environmental factors like noise or lights.
“We have a tendency, particularly in medicine, to say, ‘Well, you could do it yesterday, so you should be able to do it today,'” said Carravallah, noting that these kinds of triggers could be avoided with simple accommodations.
Another misconception may come from official diagnostic criteria which indicates “persistent deficits” are required for an ASD diagnosis. That comes with an idea that autistic people have a disability that might prevent them from doing certain jobs, she said.
“I don’t think you have to be disabled in order to be autistic. It’s a different way of thinking — it’s not a deficit,” said Carravallah, who is also an associate professor of medicine at the University of Michigan and a board-certified physician in internal medicine and pediatrics.
Empathy is also a word that comes up in conversations about autistic doctors, but Carravallah says that they can show as much empathy as people without. Misunderstandings, however, can occur and that’s something that could be addressed through accommodations.
“I think medicine’s very hierarchical, and if somebody who is above you decides that they just don’t like the way that you interact, it becomes very difficult,” Carravallah said.
Difficulties nearly led Mráček to drop out
Mráček knew med school would be challenging, especially without a formal background in science, but she felt up to it. Right away, however, she had trouble connecting with her peers.
“In tandem with that, then I’m also experiencing academic difficulty for the first time in my life.” After her first year, she took a year off for self-study to bolster her science knowledge.
It was Mráček’s fiancé, Jared Cooper, who suggested that she might consider a diagnosis of autism. He had previously spotted signs of the disorder in her father.

The nudge came after two particularly negative experiences with a supervising physician — one that Mráček says ended in a verbal confrontation — and a failed obstetrics and gynecology rotation that nearly pushed her to drop out.
“I told her then, and I still tell her now that I’ll support her no matter what and no matter what, we’ll be fine in life,” said Cooper. “If she’d quit then she quit … not because she couldn’t do it, not because she wasn’t smart enough or bright enough or brilliant enough to do it, but because it just might not have been the right fit.”
I haven’t told many people yet in pathology … because I really just feel like I fit in.”– JJ Mráček
Mráček appealed and had the failing grade on her rotation overturned. After her diagnosis, she continued with the program, eventually matching with an internal medicine program in Edmonton for her residency.
The number of patients she had to see during a single shift, the long hours, constant noise and incessant interruptions proved overwhelming.
While talking to a resident colleague in pathology, Mráček realized she might be able to use what she sees as her superpowers — that sense of justice, deep analytical skills, compassion and a strong interest in understanding the causes of disease — in another part of the hospital.
Home in pathology
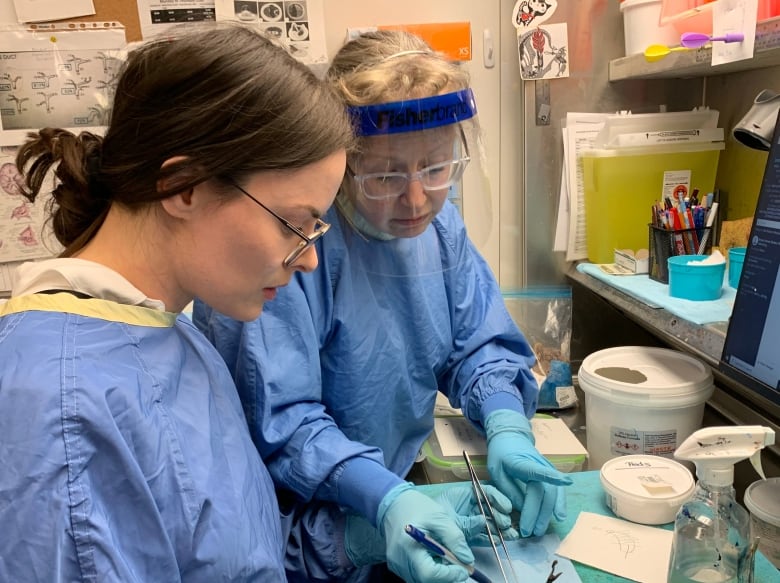
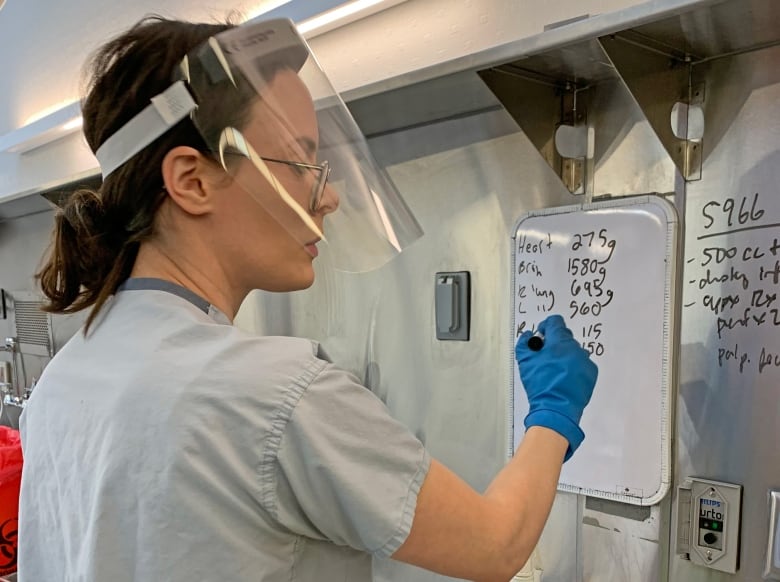
Now a resident in pathology, a department that relies on routine and structure, Mráček feels she’s found her place in medicine. Autopsies, in particular, have been a gratifying part of the work.
“I feel that I’m making something a little bit more right in the world by being a part of giving someone an answer as to why their loved one died,” she said, adding she uses her social work skills regularly in the role.
Dr. Tara Dixon, a medical examiner with the Alberta government, has been mentoring Mráček. “I’m sure you’ll be successful in your training if you carry that forward,” she told the resident on White Coat, Black Art.
Dixon says there likely isn’t enough being done to accommodate medical students and residents on the autism spectrum, but says that because the field is so broad, it can be difficult to pinpoint what and where changes need to be made.
Carravallah says it’s about recognizing that autistic people have skills — like direct communication, pattern recognition, strong ethics and a deep interest in particular topics — that are key to being a good doctor.
“People coming from different backgrounds is a really important thing,” she said. “Medicine is a team sport nowadays, so if we cut out the neurodiverse voices, we’re really going to lose a lot.”
Mráček says the associate dean of medicine at the University of Calgary encouraged her to tell colleagues and more senior doctors that she is autistic. Since then, she says she has told almost everyone.
“It’s no coincidence that ever since then, ever since I implemented his advice, I’ve had absolutely zero conflict,” she said.
“I have to think that if there’s benefit from sharing on an individual level, then I might as well take that a step further and share it to a broader audience. I think it could help a lot of people.”
There are still some people who don’t know, however.
“I haven’t told many people yet in pathology, which is funny,” she said. “I haven’t really felt the need to because I really just feel like I fit in.”

