
Scientists have discovered that a type of bacteria is not as harmless as previously thought. It can actually cause infections in patients with bronchiectasis, asthma, and chronic obstructive pulmonary disease (COPD).
An international study led by Singapore scientists discovers bacteria previously thought harmless can worsen existing lung disease.
A team of international scientists has discovered that Neisseria — a genus of bacteria that lives in the human body – is not as harmless as previously thought. In fact, it can cause infections in patients with bronchiectasis, asthma, and chronic obstructive pulmonary disease (COPD).
In a landmark study, published on September 14, 2022, in Cell Host & Microbe, the team showed conclusive evidence that Neisseria species can cause disease in the lung and are linked to worsening bronchiectasis (a type of lung disease) in patients. The scientists were led by the Nanyang Technological University, Singapore (NTU Singapore).
Bronchiectasis is a long-term condition where the airways of the lungs become abnormally enlarged for unknown reasons in up to 50 percent of Singaporean patients. The disease is up to four times more prevalent among Asians as compared to their Western counterparts and can also occur following recovery from tuberculosis.[1] In Singapore, research at Tan Tock Seng Hospital described 420 incident hospitalized bronchiectasis patients in 2017.[2] The incidence rate is 10.6 per 100,000 and increases strongly with age.
Despite its prevalence among older people, no obvious cause is found in most cases of bronchiectasis and the condition tends to arise spontaneously and without warning.[3]
To unravel the puzzle of why bronchiectasis worsens at a significantly greater rate among older Asian patients, the international team — spanning researchers and hospitals in Singapore, Malaysia, China, Australia, and the UK (see Annex) — led by LKCMedicine Associate Professor Sanjay Chotirmall, Provost’s Chair in Molecular Medicine, matched disease and infection data from 225 patients with bronchiectasis of Asian (Singapore and Malaysia) origin to those from bronchiectasis patients in Europe.
Neisseria: not so harmless after all
While Neisseria species are well known to cause meningitis and gonorrhea, they are not known to infect the lungs. Through detailed identification and meticulous characterization, the research team found that Neisseria dominated the microbiome of Asian patients with worsening bronchiectasis.
Specifically, bronchiectasis patients with predominant amounts of a subgroup of Neisseria called Neisseria subflava (N. subflava), experienced more severe disease and repeated infections (exacerbations) when compared to patients with bronchiectasis without such high amounts of Neisseria.
Upon further investigation using experimental cell and animal models, the research team confirmed that N. subflava causes cell disruption, resulting in inflammation and immune dysfunction in bronchiectasis patients with this bacterium.

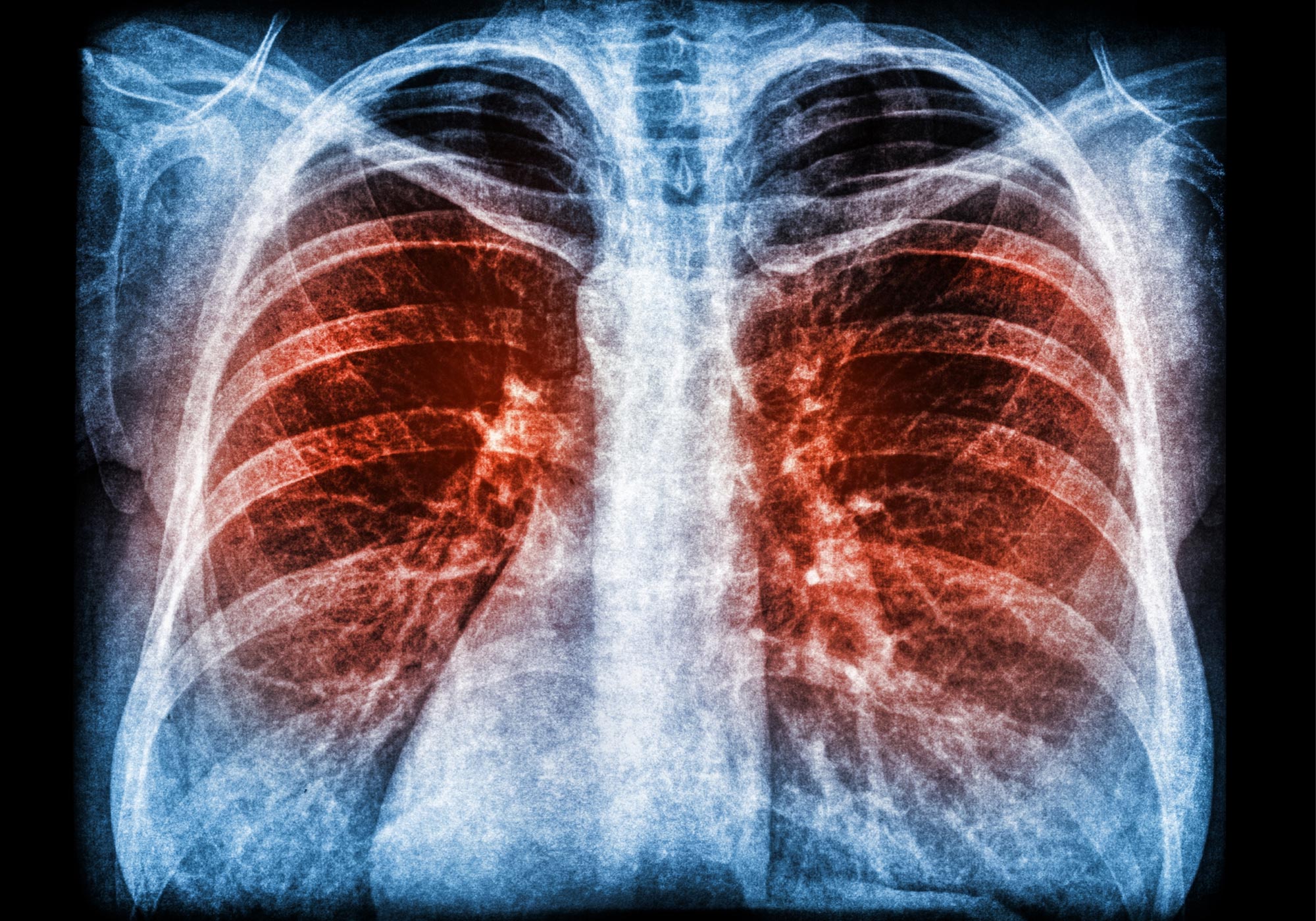
Pictured is a detection of Neisseria (N. subflava) in lung tissue from patients with bronchiectasis. Shown in red is the N. subflava detection and shown in blue is the airway cell nuclei. Credit: Cell Host & Microbe
Prior to this discovery, Neisseria was not considered to be a cause of lung infection or severe disease in bronchiectasis patients.
Lead investigator Prof Chotirmall from LKCMedicine, said, “Our findings have established, for the first time, that poorer clinical outcomes such as greater disease severity, poorer lung function, and high repeated infection rates among bronchiectasis patients are closely associated with the bacteria Neisseria and that this finding is especially important for Asian patients.”
“This discovery is significant because it can change how we treat our bronchiectasis patients with this bacterium. Doctors will now need to think about Neisseria as a potential ‘culprit’ in patients who are worsening despite treatment, and to conduct tests to identify those who may be harboring this type of bacteria in their lungs. We hope that early identification will lead to personalized therapy, and consequently, better disease outcomes for Asian patients with this devastating disease,” said Prof Chotirmall, who is also Assistant Dean (Faculty Affairs) at LKCMedicine.
This study reflects NTU’s efforts under NTU2025, the University’s five-year strategic plan that addresses humanity’s grand challenges such as human health. Conducted by international researchers from across various disciplines, the study also highlights NTU’s strength and focus on interdisciplinary research.
Broader relevance of Neisseria
Aside from linking Neisseria and severe bronchiectasis, the NTU-led research team also detected the presence of the same bacteria in other more common chronic respiratory conditions such as severe asthma and Chronic Obstructive Pulmonary Disease (COPD) – a condition that causes airflow blockage and breathing-related problems.
Using next-generation sequencing technologies, the team also sought to investigate where this bacterium may come from and sampled the homes of bronchiectasis patients with high amounts of Neisseria in their lungs. The researchers found the presence of the bacteria in the home environment, suggesting that the indoor living space and potentially the tropical climate may favor the presence of this bacteria in the Asian setting.
What is Neisseria?
The Neisseria bacteria species have been commonly identified as the cause of sexually transmitted infections like gonorrhea but also critically meningitis — an inflammation of the fluid and membranes surrounding the brain and spinal cord. Its sub-species N. subflava, however, is known to be found in the oral mucosa, throat, and upper airway of humans previously without any known link to lung infections.
This family of bacteria has always been thought of as harmless to humans, and infections caused by them have not been described – until now.
Co-author, Professor Wang De Yun from the Department of Otolaryngology at the Yong Loo Lin School of Medicine, National University of Singapore, said, “It is encouraging to see that we have made headway in identifying the Neisseria bacteria species as the cause of worsening bronchiectasis, the unlikely culprit that was originally not considered to be a threat. This comes as a strong reminder that we should not be too complacent when it comes to doing research and exercise more proactiveness in exploring various possibilities, as every seemingly innocent element could be a source of threat to our bodies and overall health.”
Co-author Andrew Tan, Associate Professor of Metabolic Disorders from LKCMedicine, said, “The reverse translational approach adopted in this work was crucial to our success. Starting from the ‘bedside’ where we studied real‐life patient experiences, we then worked backward to uncover the biological process of the bacteria. Thanks to the interdisciplinary nature of the study, the team was able to interact with members from different research disciplines, offering an enjoyable experience while gaining unique insights into the disease.”
The researchers are now looking to conduct further studies and clinical trials of Neisseria eradication from the microbiome through the newly launched LKCMedicine Centre for Microbiome Medicine, which is seeking to evaluate the benefits of targeting and treating Neisseria with antibiotics at first detection, with the hope that this will lead to better clinical outcomes for patients with chronic respiratory conditions.
Reference: “Neisseria species as pathobionts in bronchiectasis” by Liang Li, Micheál Mac Aogáin, Tengfei Xu, Tavleen Kaur Jaggi, Louisa L.Y. Chan, Jing Qu, Lan Wei, Shumin Liao, Hong Sheng Cheng, Holly R. Keir, Alison J. Dicker, Kai Sen Tan, Wang De Yun, Mariko Siyue Koh, Thun How Ong, Albert Yick Hou Lim, John A. Abisheganaden, Teck Boon Low, Tidi Maharani Hassan, Xiang Long, Peter A.B. Wark, Brian Oliver, Daniela I. Drautz-Moses, Stephan C. Schuster, Nguan Soon Tan, Mingliang Fang, James D. Chalmers and Sanjay H. Chotirmall, 14 September 2022, Cell Host & Microbe.
DOI: 10.1016/j.chom.2022.08.005
Notes
- “Trends in Bronchiectasis Among Medicare Beneficiaries in the United States, 2000 to 2007” by Amy E. Seitz, MPH; Kenneth N. Olivier, MD, MPH; Jennifer Adjemian, PhD; Steven M. Holland, MD and D. Rebecca Prevots, PhD, MPH, 1 August 2012, Chest Journal.
DOI: 10.1378/chest.11-2209 - “Epidemiology and economic burden of bronchiectasis requiring hospitalisation in Singapore” by Hwee Pin Phua, Wei-Yen Lim, Ganga Ganesan, Joanne Yoong, Kelvin Bryan Tan, John Arputhan Abisheganaden and Albert Yick Hou Lim, 12 August 2021, ERJ Open Research.
DOI: 10.1183/23120541.00334-2021 - “Geographic variation in the aetiology, epidemiology and microbiology of bronchiectasis” by Ravishankar Chandrasekaran, Micheál Mac Aogáin, James D. Chalmers, Stuart J. Elborn and Sanjay H. Chotirmall, 22 May 2018, BMC Pulmonary Medicine.
DOI: 10.1186/s12890-018-0638-0
Annex
List of collaborating institutions
- Department of Pharmacology, School of Medicine, Southern University of Science and Technology, Shenzhen, China
- Shenzhen Institutes of Advanced Technology, Chinese Academy of Sciences, Shenzhen, China
- Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore
- Biochemical Genetics Laboratory, Department of Biochemistry, St. James’s Hospital, Dublin, Ireland
- Clinical Biochemistry Unit, School of Medicine, Trinity College Dublin, Dublin, Ireland
- School of Civil and Environmental Engineering, Nanyang Technological University, Singapore
- College of Pharmaceutical Sciences, Zhejiang University, Hangzhou, China
- University of Dundee, Ninewells Hospital, Medical School, Dundee, Scotland
- Department of Otolaryngology, Infectious Disease Translational Research Programme, Yong Loo Lin School of Medicine, National University of Singapore
- Department of Respiratory and Critical Care Medicine, Singapore General Hospital, Singapore
- Department of Respiratory and Critical Care Medicine, Tan Tock Seng Hospital, Singapore
- Department of Respiratory and Critical Care Medicine, Changi General Hospital, Singapore
- Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
- Department of Respiratory Medicine and Critical Care, Peking University Shenzhen Hospital, Shenzhen, China
- Priority Research Centre for Healthy Lungs, Hunter Medical Research Institute, School of Medicine and Public Health, University of Newcastle, NSW, Australia
- Department of Respiratory and Sleep Medicine, John Hunter Hospital, New Lambton Heights, NSW, Australia
- Woolcock Institute of Medical Research, University of Sydney, Australia
- School of Life Sciences, University of Technology Sydney, Australia
- Singapore Centre for Environmental Life Sciences Engineering (SCELSE), Nanyang Technological University, Singapore
- School of Biological Sciences, Nanyang Technological University, Singapore
- Department of Environmental Science and Engineering, Fudan University, Shanghai, China

