Researchers have created a groundbreaking antibody that combines targeting, delivery, and immune activation to treat cancer, showing success in preclinical tests.
Researchers at Uppsala University and KTH Royal Institute of Technology have developed an innovative antibody-based precision medicine with the potential to treat various types of cancer.
Researchers have managed to combine three different functions in the antibody, which together strongly amplify the effect of T cells on the cancer tumor. The study has been published in Nature Communications.

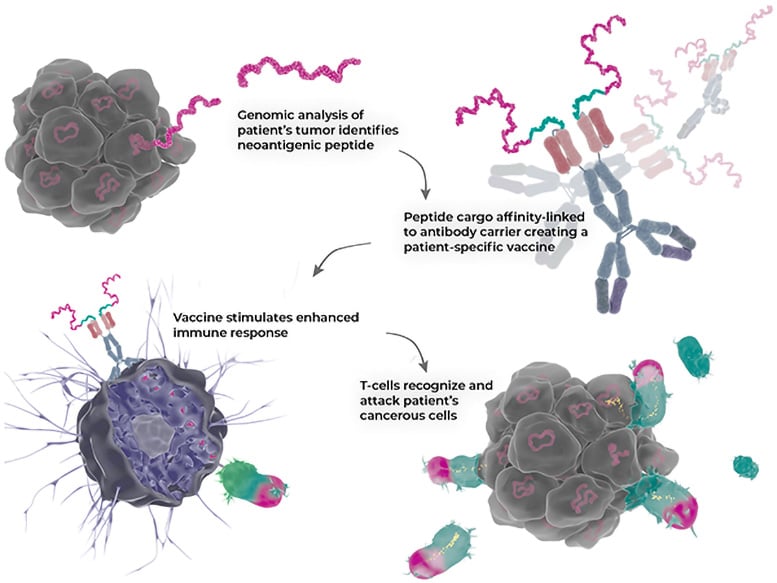
Researchers have developed a unique type of antibody that both targets and delivers a drug package via the antibody itself, while simultaneously activating the immune system (“3-in-1 design”) for personalized immunotherapy treatments.
“We have been researching precision medicine for close to 15 years now, as well as how we can use antibodies to influence an important key protein (CD40) in the immune system. We can now show that our new antibody method works as a precision medicine for cancer,” explains Sara Mangsbo, professor at the Department of Pharmacy at Uppsala University, who together with Johan Rockberg, professor at KTH Royal Institute of Technology, is the study’s lead author.
Targeting Tumor-Specific Mutations
The drug redirects the immune system to find and target specific mutations and gene changes that are only found in cancer cells, known as neoantigens. This is achieved by the new antibody both delivering the unique tumor-specific material directly to a particular type of immune cell and by stimulating this cell simultaneously, which then has the capacity to greatly enhance the T-cell response to the tumor.

The results show that the method works in several ways. Not only does it activate the right type of immune cells in human blood samples, but animal models show that mice receiving the treatment had prolonged survival and, at higher doses, also save the mice from cancer, and that the method is safer than previous cancer treatments the researchers have studied.
Customized precision medicines can be both costly and time-consuming to develop.
“The advantage of our drug is that it is easy to produce on a larger scale, yet can be easily tailored to the patient’s disease or specific tumor. The medicine consists of two parts that are combined, a targeting bispecific antibody – which can be produced in large quantities in advance – and a custom peptide part, which is produced rapidly synthetically on a small scale for a desired type of cancer. Both in terms of production cost and the short time it takes to tailor a peptide to a new tumor, this increases availability and should make it quicker for patients to go from diagnosis to treatment,” explains Johan Rockberg, Professor at KTH Royal Institute of Technology.
The aim of the study was to establish a more flexible, faster, and safer treatment for cancer than those currently available. The study has already shown that the method has the potential to be customized for each patient, thereby strengthening the immune system against cancer. The next step is to use the fully optimized production process to manufacture the drug candidate for further safety studies and then start clinical trials in humans.
Reference: “A bispecific CD40 agonistic antibody allowing for antibody-peptide conjugate formation to enable cancer-specific peptide delivery, resulting in improved T Cell proliferation and anti-tumor immunity in mice” by Aman Mebrahtu, Ida Laurén, Rosanne Veerman, Gözde Güclüler Akpinar, Martin Lord, Alexandros Kostakis, Juan Astorga-Wells, Leif Dahllund, Anders Olsson, Oscar Andersson, Jonathan Persson, Helena Persson, Pierre Dönnes, Johan Rockberg and Sara Mangsbo, 5 November 2024, Nature Communications.
DOI: 10.1038/s41467-024-53839-5
Funding: Knut och Alice Wallenbergs Stiftelse, Vinnova, Swedish Cancer Society, Strike Pharma

