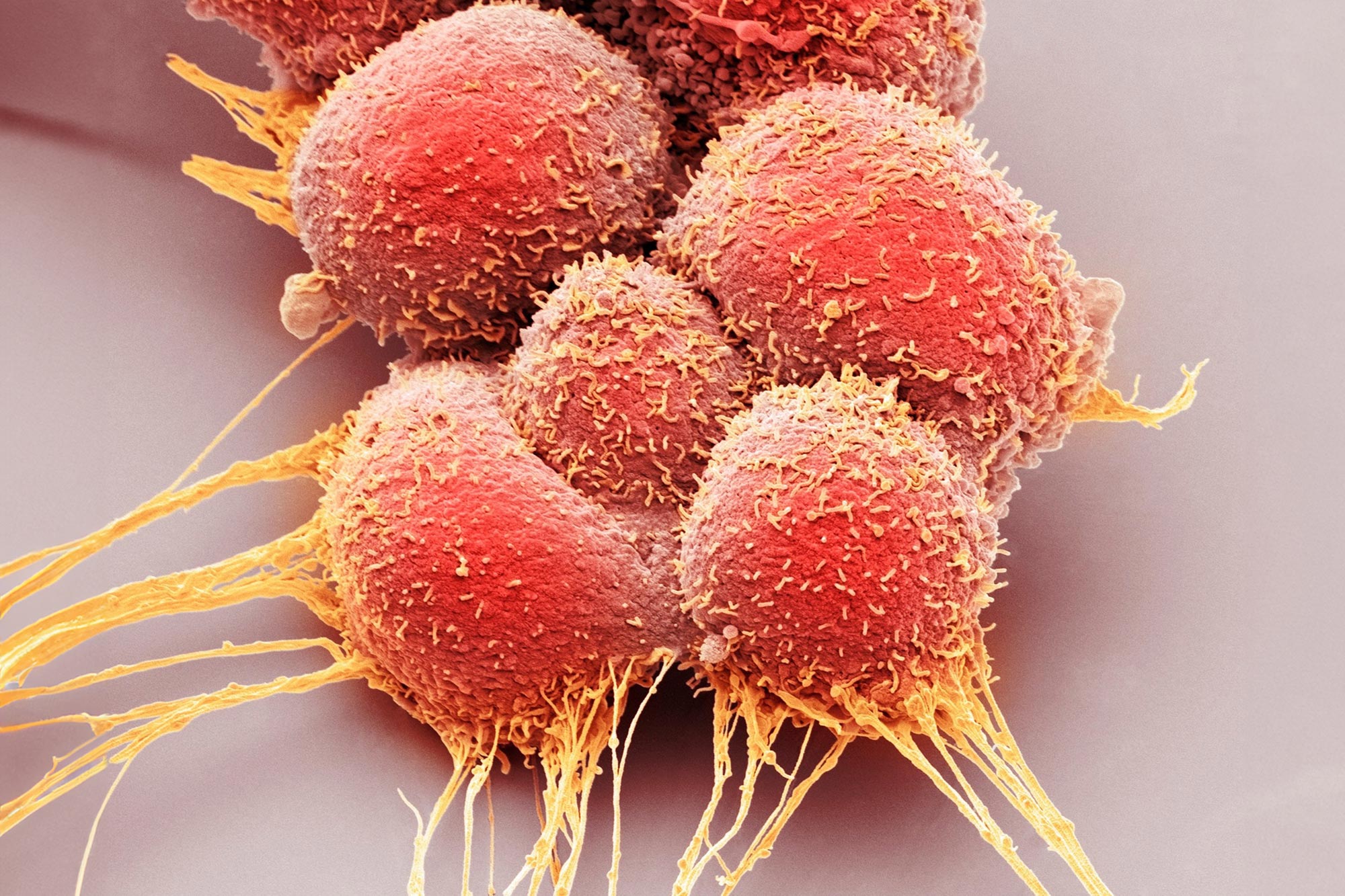
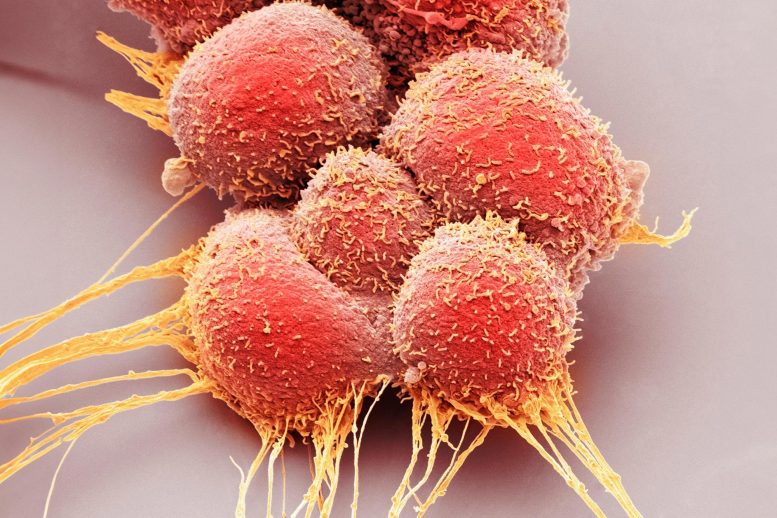
gemA groundbreaking approach slows tumor growth while boosting the immune system’s defense against cancer cells.
Prostate cancer ranks as the second most common cancer among men globally. Despite recent medical advancements, this form of cancer continues to account for one in eight male cancer-related deaths in Austria.
An international research team led by MedUni Vienna has now investigated a new strategy for the development of treatment options that not only slow tumor growth, but also stimulate the immune system to combat tumor cells. The results of the study have just been published in the top journal Molecular Cancer.
The scientific team focused its investigations on the GP130 signaling pathway, which researchers expect to have a major potential in the fight against cancer. The background: the signaling pathway, which is mediated by the protein GP130, plays a central role in cell communication and influences the activity of the transcription factor STAT3, which in turn is associated with the development and spread of tumors.
Accordingly, blocking the GP130 signaling pathway is currently seen as a great hope in cancer medicine. Yet the current study proves the opposite: tumor growth can be slowed down not by inhibiting but by activating the GP130 signaling pathway in prostate cells.
New hope, especially for aggressive tumors
To achieve these new findings, the researchers investigated genetically modified mice in which GP130 was specifically activated in the prostate. “This allowed us to directly observe the reduction in tumor growth in the cell,” reports Lukas Kenner (Clinical Department of Pathology, MedUni Vienna), who led the study together with Stefan Rose-John (Biochemical Institute, University of Kiel). The results were further backed up by analyses of tissue samples from prostate cancer patients. This showed that high GP130 values correlate with a better survival rate. At the same time, extensive molecular analyses were carried out, including gene expression profiling.
“Our research provides exciting new evidence that the activation of GP130 in prostate cells not only slows tumor growth, but also stimulates the immune system to actively fight the cancer cells,” says Lukas Kenner, summarising the significance of the results, which will now be confirmed in further studies. The research work opens up a promising new therapeutic option, particularly for aggressive prostate cancer, which is still difficult to treat.
Reference: “Cell-autonomous IL6ST activation suppresses prostate cancer development via STAT3/ARF/p53-driven senescence and confers an immune-active tumor microenvironment” by Christina Sternberg, Martin Raigel, Tanja Limberger, Karolína Trachtová, Michaela Schlederer, Desiree Lindner, Petra Kodajova, Jiaye Yang, Roman Ziegler, Jessica Kalla, Stefan Stoiber, Saptaswa Dey, Daniela Zwolanek, Heidi A. Neubauer, Monika Oberhuber, Torben Redmer, Václav Hejret, Boris Tichy, Martina Tomberger, Nora S. Harbusch, Jan Pencik, Simone Tangermann, Vojtech Bystry, Jenny L. Persson, Gerda Egger, Sarka Pospisilova, Robert Eferl, Peter Wolf, Felix Sternberg, Sandra Högler, Sabine Lagger, Stefan Rose-John and Lukas Kenner, 31 October 2024, Molecular Cancer.
DOI: 10.1186/s12943-024-02114-8

