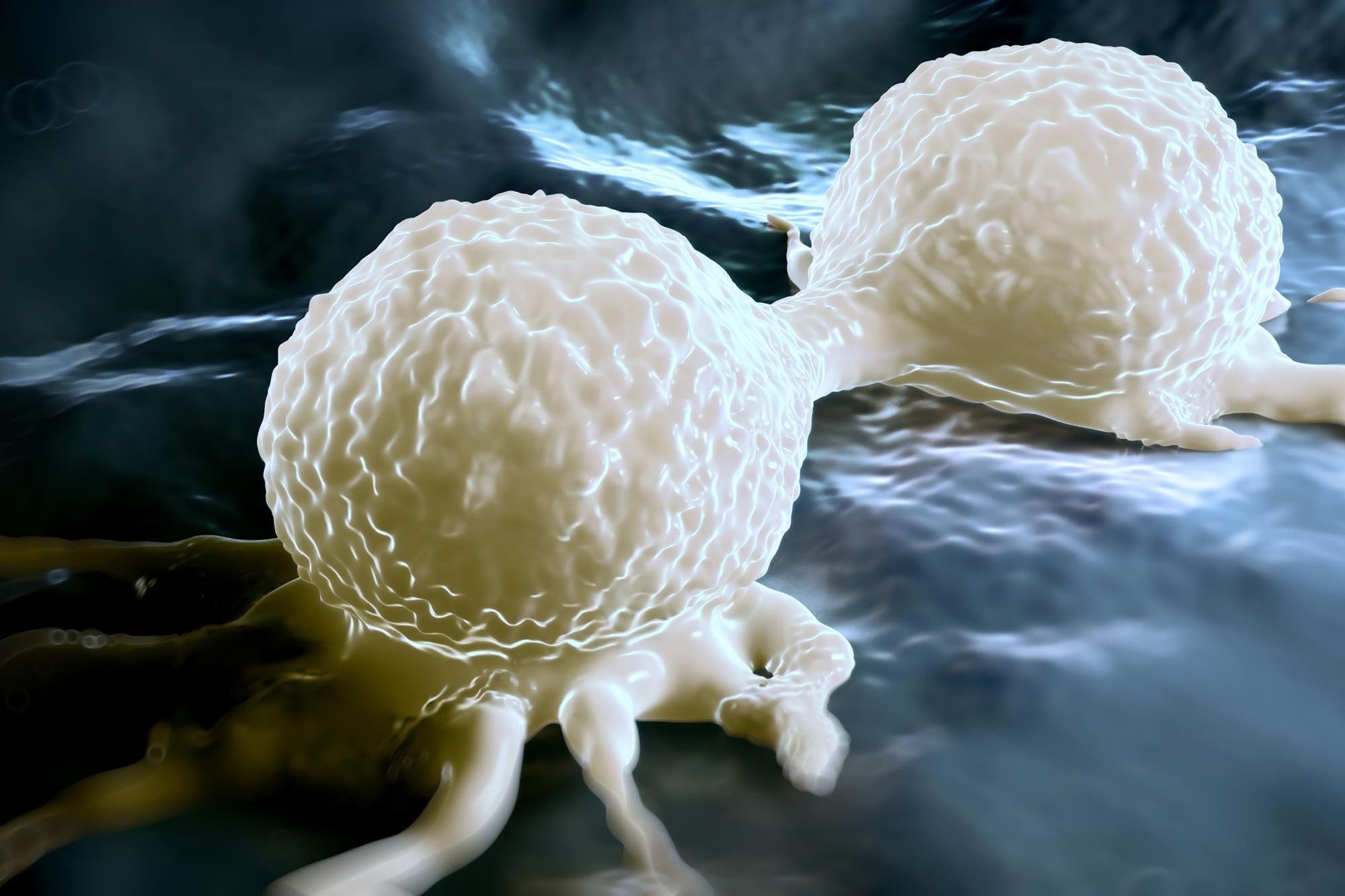
The hormone decreases a type of white blood cell that helps keep tumors in check; restricting the hormone could be a therapeutic approach.
A new study from Duke Cancer Institute unveils that estrogens facilitate the growth of multiple cancer types, including breast cancers without estrogen receptors, by weakening the immune response and diminishing immunotherapy effectiveness. Anti-estrogen treatments were found to counteract these effects, enhancing the effectiveness of cancer immunotherapies across various cancers.
Estrogens and Cancer Growth
Estrogens are known to drive tumor growth in breast cancer cells that carry its receptors, but a new study by Duke Cancer Institute researchers unexpectedly finds that estrogens play a role in fueling the growth of breast cancers without the receptors, as well as numerous other cancers.
In a paper published today (September 27) in the journal Science Advances, the researchers describe how estrogens not only decrease the ability of the immune system to attack tumors, but also reduce the effectiveness of immunotherapies that are used to treat many cancers, notably triple-negative breast cancers. Triple-negative breast cancers are an aggressive form of disease that are negative for estrogen, progesterone, and the HER2 receptor proteins
Enhancing Immunotherapy Efficacy
Informed by retrospective analysis of patient data and experiments in mice, the researchers found that anti-estrogen drugs reversed the effects of estrogens, restoring potency to immunotherapies.
“The treatment for triple-negative breast cancer has been greatly improved with the advent of immunotherapy,” said senior author Donald McDonnell, Ph.D., professor in the departments of Medicine, Pharmacology and Cancer Biology, and Cell Biology at Duke University School of Medicine.
“Developing ways to increase the anti-cancer activity of immunotherapies is a primary goal of our research,” McDonnell said. “Here we have found a simple way bolster the effectiveness of immunotherapy for this type of breast cancer and the benefit was even seen in other cancers, including melanoma and colon cancers.”
Targeting White Blood Cells in Cancer
McDonnell and colleagues, including lead author Sandeep Artham, a postdoctoral associate in the McDonnell lab, focused on a type of white blood cell called eosinophils, which are typically activated during allergic reactions and inflammatory diseases.
Eosinophils have recently been identified as important in tumors, and a phenomenon called tumor associated tissue eosinophilia, or TATE, is associated with better outcomes among patients with multiple types of cancer, including colon, esophageal, gastric, oral, melanoma, and liver cancers.
Hormonal Impact on Tumor Growth
In their studies, the Duke team described how estrogens decrease the number of eosinophils and TATE in mice. The hormone contributes to increased tumor growth in estrogen receptor-negative breast cancer tumors and in melanoma tumors, which do not rely on estrogen receptors for tumor growth.
Conversely, anti-estrogen therapies inhibited estrogen receptor signaling and enhanced the efficacy of immunotherapies, slowing tumor growth.
Clinical Implications and Future Directions
“These findings highlight the importance of estrogen-receptor signaling as a regulator of eosinophil biology and TATE and highlight the potential near-term clinical application of anti-estrogen drugs to increase the benefits of immunotherapies in multiple tumor types,” McDonnell said.
He said clinical trials are being planned using an investigational anti-estrogen drug called lasofoxifene among patients with triple-negative breast cancers.
Reference: 27 September 2024, Science Advances.
In addition to McDonnell and Artham, study authors include Patrick K. Juras, Aditi Goyal, Prabuddha Chakraborty, Jovita Byemerwa, Siyao Liu, Suzanne E. Wardell, Binita Chakraborty, Daniel Crowder, Felicia Lim, Corinne H. Strawser, Madeline Newlin, Alessandro Racioppi, Susan Dent, Babak Mirminachi, Jatin Roper Charles M Perou, and Ching-Yi Chang.
The study received funding support from the Department of Defense Innovator grant (W81XWH-18-1-0064), the National Institutes of Health (R01CA276089, RO1-CA148761) and the National Cancer Institute Breast SPORE program (P50-CA058223).