A study on mice demonstrates that engineered immune cell therapy safeguards damaged neurons.
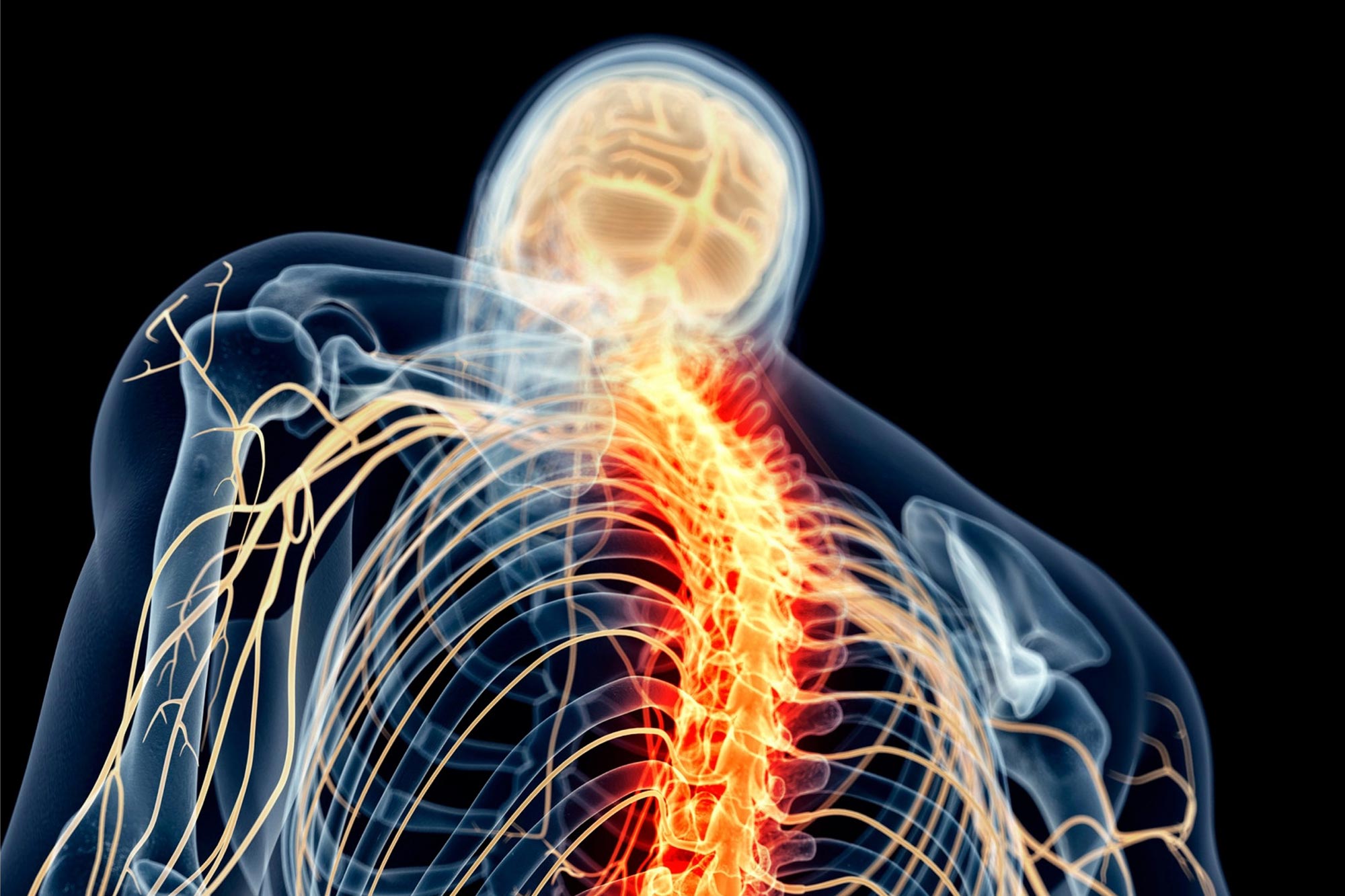
Severe spinal cord injuries harm nerve cells, breaking the communication link between the brain and the rest of the body, and resulting in permanent disabilities for millions globally. The initial injury is only a small part of the total harm to the spinal cord, a tissue extending from the brain stem to the lower back. Much of the damage results from degenerative changes that occur at the site of the injury.
While there is substantial research into developing interventions to repair injured tissue, scientists at Washington University School of Medicine in St. Louis focused instead on developing, in mice, an immunotherapy to minimize the damage from traumatic spinal cord injury. Their findings show that immunotherapy can lessen such damage by protecting neurons at the injury site from being attacked by immune cells.
The study, published in Nature, demonstrates success in mice given the immunotherapy and presents a novel approach with the potential to help improve outcomes for people recovering from spinal cord injuries.
Understanding the Role of Immune Cells
“Immune cells in the central nervous system have a reputation for being the bad guys that can harm the brain and spinal cord,” said senior author Jonathan Kipnis, PhD, the Alan A. and Edith L. Wolff Distinguished Professor of Pathology & Immunology and a BJC Investigator at WashU Medicine. “But our study shows that it’s possible to take advantage of immune cells’ neuroprotective function, while controlling their inherent detrimental abilities, to help in the recovery from central nervous system injury.”
Shortly after injury to the nervous system, immune cells flood the site. Among them is a mixture of activated T cells – a subset of immune cells – that either harm or protect the surrounding neurons. Wenqing Gao, PhD, a postdoctoral research associate in the Department of Pathology & Immunology and the study’s first author, analyzed T cells from the spinal cords of injured mice and performed a genetic analysis to decode their identities. Her goal was to separate the harmful from the protective T cells and create numerous copies of the beneficial cells with which to treat the injured mice.
But there was a catch, she found. The protective T cells that swoop into the injury site can mistakenly attack the body’s surrounding tissues when activated for too long, causing autoimmune disease. To improve the therapy’s safety, Gao modified the cells to shut off after a few days.
Promising Results and Future Goals
Mice given the modified T cells had better mobility than did the untreated mice. The researchers saw the biggest improvements when the mice were infused with T cells within a week of the injury. None of the mice receiving immunotherapy developed a destructive autoimmune reaction.
“There are no effective treatments for traumatic injuries to the central nervous system,” explained Gao. “We developed immunotherapy for such injuries by taking advantage of the protective immune cells that infiltrate the injury site and found that it dramatically improved mobility in mice.”
In collaboration with WashU Medicine’s Wilson Zachary Ray, MD, a spinal cord surgeon and the Henry G. & Edith R. Schwartz Professor of Neurosurgery, the researchers also looked every day for a week for T cells in the cerebral spinal fluid of patients with spinal cord injuries. They found a significant expansion of the T cells, confirming the feasibility of expanding protective T cells from such patients to generate the immunotherapy.
“Our future goal is to devise a clinical trial to test the therapy in people with such injuries, while expanding this work to neurodegenerative diseases such as amyotrophic lateral sclerosis (ALS) as well as Alzheimer’s and Parkinson’s diseases,” Gao said.
Added Kipnis: “Although the initial trigger in neurodegenerative diseases is different, the subsequent death of neurons may very well be mediated by similar processes, opening an opportunity for adapting our engineered cells for use as a therapy in neurodegeneration.”
Reference: “Engineered T cell therapy for central nervous system injury” by Wenqing Gao, Min Woo Kim, Taitea Dykstra, Siling Du, Pavle Boskovic, Cheryl F. Lichti, Miguel A. Ruiz-Cardozo, Xingxing Gu, Tal Weizman Shapira, Justin Rustenhoven, Camilo Molina, Igor Smirnov, Yifat Merbl, Wilson Z. Ray and Jonathan Kipnis, 4 September 2024, Nature.
DOI: 10.1038/s41586-024-07906-y
This work was supported by the BJC Investigators Program at WashU.