
White Coat Black Art26:30The Trouble with Home Care (Part 1)
Kirsten and David MacDonald’s lives were both changed forever last year when Kirsten was diagnosed with amyotrophic lateral sclerosis (ALS), and David became her full-time caregiver.
“A year and a half ago, Kirsten could run 5K, no problem. And so in the course of a year and a half now, she has absolutely no use of her feet, and her arms and her legs. And her voice is going. She’s about a week away from being non-verbal,” David told White Coat, Black Art‘s Dr. Brian Goldman during a visit to their home in Ontario’s Muskoka region in August.
David, 61, has put his business on hold. Now he spends 14 hours a day caring for Kirsten, who is 55, in addition to caring for their six-year old child.
One hope for the MacDonalds is home care, provided by occupational therapists and personal support workers (PSW) paid by the province.
A central agency evaluated their need and approved them for home-care help — but the actual hours they get is dependent on staff availability.
The MacDonalds are currently getting eight hours of PSW home care a week — half of what they were approved for.
“I think it’s incredibly horrible,” said Kirsten. “I mean, I’m in a very good position with a caring husband, but I can’t imagine what other people are going through.”
Several patients, home care providers and medical experts who spoke with White Coat, Black Art all agree that a rethink to home care is needed in Canada.
If not, they warn, the current shortcomings will be felt more acutely, and add further pressure to ERs, hospitals and long-term care homes already under massive stress.
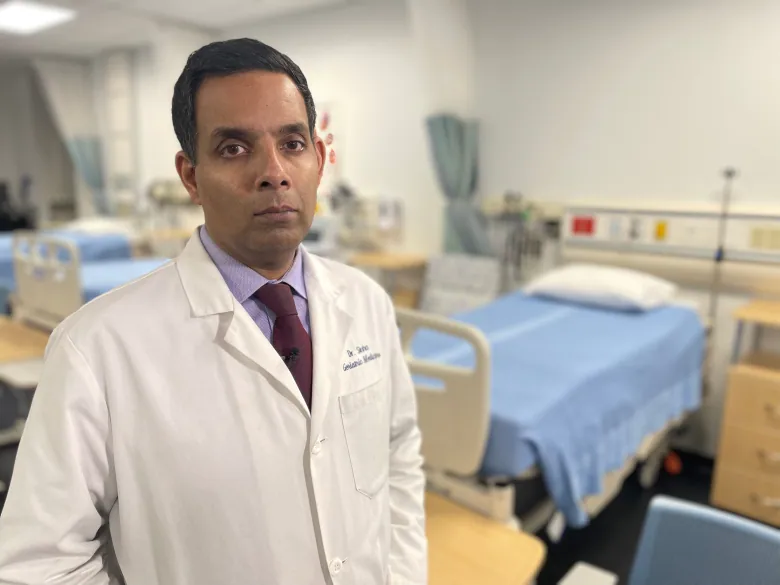
“Whatever we do have across our provinces and territories, it’s funded based on maybe politics and necessity, as opposed to really seeing home care as a vital part of our system,” said Dr. Samir Sinha, director of geriatrics at Sinai Health and the University Health Network in Toronto, who is developing a national seniors strategy for the National Institute on Ageing.
White Coat Black Art26:29The cure for home care
The wait list grows
According to the Canadian Medical Association, nearly one million Canadians today rely on some form of home care. Another half million are expected to need it by the end of the decade. And by 2031, overall home care costs are expected to double.
Caryn Farnsworth, an occupational therapist (OT) based in Huntsville, Ont., helps the MacDonalds on an as-needed basis.

She does her best to help the situation in the few hours she’s able to be there. During her visit with Dr. Goldman present, she asks Kirsten how many “good days” she’s had lately — a lot of them, Kirsten replies.
She helps David carry a brand-new commode, which she dubs “the Cadillac of commodes,” down to the main floor of their home.
Like any other visit, it ends before long, and she’s on her way to visit another of her more than 80 clients scattered across the province’s Muskoka region.
Farnsworth spends about three to five hours a day — half of her work week — travelling between clients’ homes. The wait list to see her can be as long as a year.

As one of only two OTs in her agency serving the region, Farnsworth’s energy and resources are stretched thin. Rising gas prices have only put more pressure on her expenses.
“It’s exceptionally frustrating. I feel that home care is an essential part of our medical system that just doesn’t seem to get the funding and the care that the people in the community need,” Farnsworth said.
‘I really want to stay at home’
Another of Farnsworth’s clients, 52-year-old Hali Camick, lives in Kilworthy, Ont., a hamlet northeast of Sparrow Lake. She has severe multiple sclerosis, and a bout of COVID-19 has made things worse.
As a Mohawk woman from the Wahta First Nation, she qualifies for Non-Insured Health Benefits for First Nations and Inuit. But it’s not enough.

“I really want to stay at home. I have a son with special needs, and he’s with me too. Mum moved in a year ago, so she’s not getting any younger, either,” she said. “The more help I can get would be great.”
“These stories break my heart because I hear them all the time,” said Sinha.
He worries that as people spend more and more time on wait lists, their families can burn out caring for their loved ones when they don’t have the help of providers like Farnsworth and personal support workers — which is most of the time.
The Dutch ‘Buurtzorg’
Zayna Khayat, a futurist and adjunct professor at the Rotman School of Management at the University of Toronto, recently drafted a pilot of a Canadian home-care model inspired by the Buurtzorg, the name of both a system and a non-profit in the Netherlands.
The word Buurtzorg translates to “neighbourhood model.” In Khayat’s pilot, a patient’s care plan would be decided by their family members and nurse, rather than a central government agency.

Khayat says Ontario officials were on board, but interest and funding fell through as home care visits dropped off during the beginning of the COVID-19 pandemic.In the Netherlands, the Buurtzorg is nimble enough to provide more time with a patient when they need help the most, and scale that back when it’s not necessary, Khayat explained.
“They then get given a budget based on the needs of the patient…. As long as they hit the results, they decide how they want to orchestrate and use the budget,” she said.
Eventually, she hopes, “it’ll be very unusual to go to these places called clinics and hospitals to get care, just like you don’t [often] go to the bank to get cash anymore.”
Khayat says the overall cost of the Buurtzorg model can cost more than a traditional home-care model, but argues it produces better results.
In her view, it’s more cost-effective as it eliminates management-level expenses in favour of paying higher wages to the direct home-care providers themselves.
The Denmark model
Sinha said wage parity for health-care providers, which is offered in Denmark, could provide part of the solution to that problem.
“No matter where you work — as a personal support worker, as a nurse — number one, you’re actually paid a respectful wage, which is important,” he explained.

In the 1980s, Denmark redirected support from building new nursing homes to investing in home care. CBC Marketplace travelled to Denmark with Sinha earlier this year for a closer look at their health-care model.
Denmark, Sinha explains, spends about twice as much on long-term care services than Canada. About two-thirds of that is spent on home care, with the final third on nursing-home care.
“Canada’s the opposite,” he said. “We spend two thirds of our spending on warehousing people in homes and only a third about keeping them in their own homes.”
Cost of care
Following Denmark’s example, Sinha argues, would be less expensive for Canada than continuing to build and plan long-term care homes.
“Our own Ministry of Health in Ontario has said that caring for a person in their own home, for example, who is long-term care eligible, costs them about $100 a day. Caring for them in a long-term care home, about $200 a day. And if they are stuck in hospital waiting for a long term care bed, it’s about $750 a day,” he said.
In a statement to CBC Radio, Ontario’s Ministry of Health reiterated previous commitments, including investing $1 billion over three years to home care and establishing Ontario Health Teams (OHTs) to provide “a new model of integrated care delivery” that includes home and community care.
David and Kirsten MacDonald are doing the best they can to get by. But the costs of that care has run into the thousands of dollars, even with help from the ALS society — including installing two chairlifts in their home, the aforementioned commode, and a mechanized lift Kirsten must use, with assistance, to get on and off the commode.
It’s only a matter of time until David is forced to call 911 and rush Kirsten to the nearest hospital.
Produced by Amina Zafar and Colleen Ross.

