This story is part of CBC Health’s Second Opinion, a weekly analysis of health and medical science news emailed to subscribers on Saturday mornings. If you haven’t subscribed yet, you can do that by clicking here.
In mid-July, when Doug Moore’s daughter fell and hurt her wrist at the family’s property in northern B.C., he rushed the nine-year-old to the nearest hospital — only to find the emergency department had shut down.
There was no advance notice of the closure, the Fort St. John resident recently told CBC’s Daybreak North.
“When you’ve got a nine-year-old, and it’s 9:30 at night, and she’s tired, she’s in pain … it definitely makes me nervous for my family and for those around us,” he said.
Northern B.C. has been hit hard by emergency closures again this summer. Between July 22 to July 28, there was at least one ER service interruption per day in the northern half of the province, prompting rallies in parts of the region.
The ER at the largest hospital in the area — serving nearly 30,000 residents — was shuttered five times in just one week.
But the crisis is also playing out country-wide, with no clear solutions in sight.
“There continue to be just unprecedented numbers of emergency department closures,” said Natalie Mehra, executive director of the Ontario Health Coalition, an advocacy group that released last year’s headline-making tally of shutdowns in the province.
That 2023 report found there were close to 870 emergency department closures across Ontario that year — an all-time high — and Mehra said her team’s early data for 2024 shows a similar trend.
“Up until a few years ago,” she said, “we’d never seen anything like that.”
Parts of Alberta, Quebec, P.E.I. and beyond are also reporting ER closures, and they’re usually linked to staff shortages. This persistent issue is prompting a flurry of potential remedies, from extensions to locum programs meant to bring in temporary staff, to virtual ERs that combine online assessments with in-person patient care.
Yet many medical experts warn constant closures of Canadian emergency departments are merely a symptom of bigger issues throughout the country’s strained health-care system, and won’t be an easy fix.
“It’s just getting to a tipping point where you just don’t have enough people willing and able to provide the coverage anymore,” said Dr. Gord McInnes, president of the emergency medicine section for the Doctors of BC, a voluntary medical association representing physicians and medical students.
Staff shortages, lack of primary care
On one hand, the problems plaguing ERs across the country mainly come down to simple supply and demand: There’s a constant influx of patients seeking care, and — particularly after the pressures of the COVID-19 pandemic — an ongoing shortage of health-care professionals available.
But McInnis stressed the factors at play can be layered and tough to untwine, and exist far beyond ERs themselves. Patient needs are increasingly complex as the country’s population grows and ages, all while the health-care system is facing pressures on several fronts.

“One of the big problems is our lack of primary care,” McInnis said.
Data from the OurCare initiative suggests the number of Canadians without regular access to a primary care provider, like a family doctor or nurse practitioner, jumped from 4.5 million in 2019 before the pandemic to an estimated 6.5 million last year.
So where do those Canadians go for both urgent and routine care? Other figures suggest they’re increasingly ending up in emergency departments.
There were roughly one million more unscheduled ER visits in 2022-2023 compared to the year before, according to the Canadian Institute for Health Information.
Pandemic burnout
ERs are facing specific pressures of their own, in part tied to pandemic-related burnout that’s led to an exodus of health-care workers.
To combat that, multiple provinces rely on locum programs, which bring in temporary physicians to fill shifts, and pay them a premium for it.
In Ontario, a rolling locum program first launched in the pandemic has been extended beyond its March expiry date, but only until the end of September. The province also recently announced $10 million in funding to help more than 1,000 nurses train in emergency department care.
Last month, B.C. Health Minister Adrian Dix also told CBC News that hiring efforts, hundreds of additional seats for nursing training programs, and a locum program are all mitigating that province’s hospital staffing crunch — with locums and incentives helping to identify and fill more than 1,100 shifts in the previous three months.
A union representing Ontario health-care workers has released survey data highlighting the stress, exhaustion and burnout experienced by hospital workers — with many considering a new career path. The union is calling for more provincial funding to ease the worsening staffing crisis.
Bottlenecks in health-care system remain
Still, multiple health-care advocates agreed those ER-focused efforts are merely a stopgap, and don’t get to the root of the issue.
One key problem is the bottlenecks elsewhere in the health-care system, including the long-term issue of patients being stuck in hospital beds while waiting for other types of care in the community.
“We simply have not got sufficient physicians and nurses to staff many of these shifts, and there are challenges in overcrowding,” said Dr. Kathleen Ross, co-president of the Canadian Medical Association (CMA), a national association representing physicians.
Those challenges are linked to both patients filling ERs due to the lack of primary care, she explained, along with backlogs elsewhere in hospitals.
“Can we move people to the ward? Can we have people access care in the community? Is there home care support so we can manage patients at home? All of these things are intersecting to land us where we are today.”
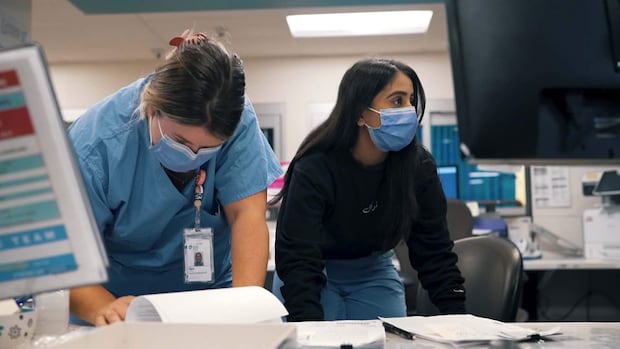
For The National, a CBC News crew gets rare access to three rural Ontario emergency rooms to see how they’re fighting to care for patients and keep the doors open despite chronic staff shortages.
Are virtual ERs a solution?
In Newfoundland, officials are trying another approach: Virtual ERs.
The province signed a multimillion-dollar contract with an American company last November to help provide virtual staffing at rural emergency departments. It’s now in use at the 12-bed hospital in New-Wes-Valley, a 2,000-person town on the northeastern coast.
The move is controversial, and comes with a downside for patients, acknowledged the town’s mayor and a former paramedic, Mike Tiller, in a recent call with CBC News.
“When they go to the virtual care, they may get a doctor from England one week, they may get a doctor from somewhere in Canada another week, and you’re not getting that continuity of care,” he said.
But it’s better than ERs being shuttered entirely, Tiller stressed, since the initial virtual assessment fills a staffing gap.
The approach may already be saving lives, he added: One patient who arrived at the town’s hospital in heart distress was able to quickly get life-saving blood clot-busting medication, thanks to a virtual doctor working in collaboration with the on-site health-care team.
“Had the hospital been on diversion at the time, that person would have had to travel an extra hour and 15 minutes just to get the initial assessment,” he said. “And, you know, may not have made it.”
Doctors in multiple provinces are sounding the alarm over long waits and over-capacity hospitals as respiratory illnesses spike and medical staff are overworked. Some are even warning some patients to stay away from the ER.
‘Pushed to the brink’
Others like Dr. Trevor Jain, the Charlottetown-based spokesperson for the Canadian Association of Emergency Physicians, questioned how outsourcing care to a virtual physician can even count as a functioning ER.
“Unless you have an emergency physician and an appropriately staffed emergency department that can resuscitate the most sick Canadians in their most time of need, that’s not an emergency department,” he said.
Jain said what’s needed now are broader investments in emergency care, since the crisis is starting to spill from remote and rural regions into urban centres that are also feeling the strain of higher patient demand.
“If we don’t invest in emergency physicians, emergency RNs and emergency departments, you’re going to see even more closures,” he said.
Ross, speaking for the CMA, stressed there’s no one-size-fits-all solution to such a widespread and ongoing problem. Instead, it’ll take a combination of efforts to curtail the pressures on ERs themselves and reduce the broader overcrowding in Canadian hospitals.
“It highlights for us how fragile the health-care system truly is — and really pushed to the brink.”