The WHO Director-General, Tedros Adhanom Ghebreyesus, called for the meeting last Wednesday to seek advice on whether the mpox – previously monkeypox – outbreaks are cause for international concern.
On Tuesday, the Africa Centres for Disease Control and Prevention (CDC) declared the situation a public health emergency.
“The Emergency Committee’s advice to me, and that of the [Africa CDC], which yesterday declared a public health emergency of regional security, are aligned,” Tedros said in a post on the social media platform X, formerly Twitter.
Mpox cases have been spreading throughout many countries in Africa, particularly the Democratic Republic of the Congo (DRC) and neighbouring Burundi, Kenya, Rwanda and Uganda. The potential for further spread in Africa is worrying, said the WHO chief.
“In addition to other outbreaks of other clades of mpox in other parts of Africa, it’s clear that a coordinated international response is essential to stop these outbreaks and save lives,” Tedros said.
This year already saw over 14,000 reported cases of the virus with 524 deaths, a significant increase in reported cases from 2023.
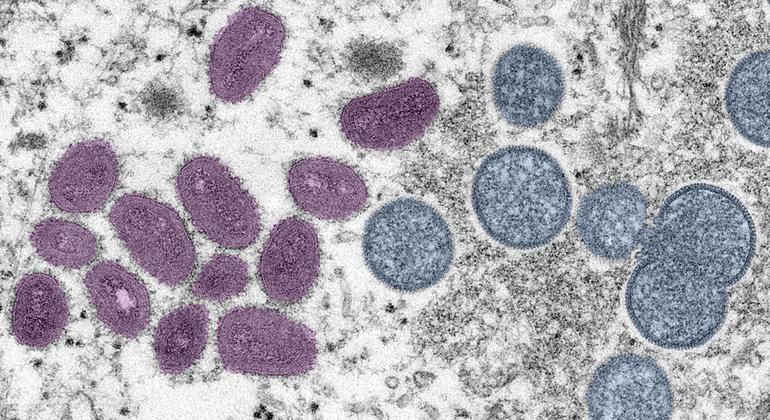
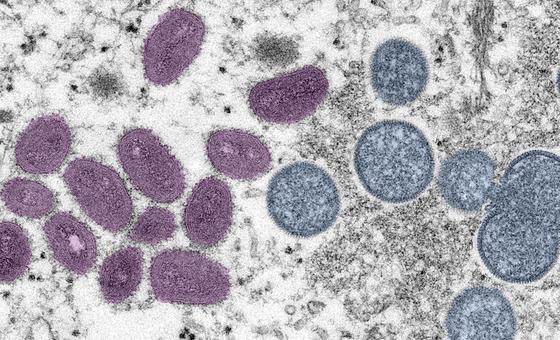
Tedros previously mentioned that the mpox outbreaks have occurred due to different viruses called clades.
At Wednesday’s meeting, he said there was transmission of the so-called clade 1b virus in the DRC last year which was caused “mainly through sexual networks”. This clade is reportedly deadlier and more easily transmitted from person to person.
Clade 1 has been circulating in the DRC for years while clade 2 was responsible for the global outbreak of 2022 which was declared an international public health emergency.
Tedros said in the past month that around 90 cases of successor clade 1b were reported in countries neighbouring the DRC which had not reported mpox cases before.
“Stopping these outbreaks will require a tailored and comprehensive response, with communities at the centre, as always,” Tedros said.
Addressing outbreak drivers
The WHO chief said the UN agency is working with governments of the affected countries, the Africa CDC and other partners to “understand and address the drivers of these outbreaks”.
“For example, we are providing machines to analyse blood samples and confirm cases of mpo [and] supporting laboratories to sequence viral samples,” he said.
He further mentioned “supporting case investigation and contact tracing” on the ground, training for health care workers and much more.
WHO regional response
“WHO has developed a regional response plan, requiring an initial $15 million to support surveillance, preparedness and response activities,” Tedros said.
This response was funded by $1.45 million from the WHO Contingency Fund for Emergencies.
More funds will be released in the coming days and the WHO chief is also appealing for more donor support.
Emergency vaccines
Currently, two WHO-recommended and approved vaccines are being used to combat the mpox virus outbreak.
Under an Emergency Use Listing (EUL) call last week, Tedros also invited manufacturers of mpox vaccines to express interest in producing them to “accelerate vaccine access for lower-income countries which have not yet issued their own national regulatory approval”.
EUL will allow partners like the UN Children’s Fund (UNICEF) to gather vaccines for distribution.
“We are working with all partners to facilitate equitable access to diagnostics, vaccines, supplies for clinical care and other tools,” Tedros said.
WHO recommendations
Last August, the WHO chief released standing recommendations under the IHR to monitor mpox cases.
These recommendations were set to expire in five days, on 20 August 2024, but will be extended for another year to “support countries to respond to the chronic risk of mpox”.
Some of the recommendations include enhancing community protection through adapting public health and social measures to local contexts, providing guidance and resources for delivering clinical mpox care and more.
Tedros said WHO is “committed in the days and weeks ahead to coordinate the global response, working closely with each of the affected countries and leveraging our on-the-ground presence to prevent transmission, treat those infected and save lives”.