To diagnose and treat Alzheimer’s disease effectively, doctors say they need affordable and accessible tests to screen people at midlife and then stave off symptoms. Here’s where researchers are at for the first step.
About 750,000 Canadians live with Alzheimer’s disease or another form of dementia. Alzheimer’s is the most common form, with symptoms such as memory loss, changes in judgment and mood or problems with language that are irreversible and eventually fatal.
Families and their physicians have long sought a blood test to accurately predict the development of Alzheimer’s in people with memory problems in the hopes that early diagnosis and existing treatments could at least slow worsening symptoms.
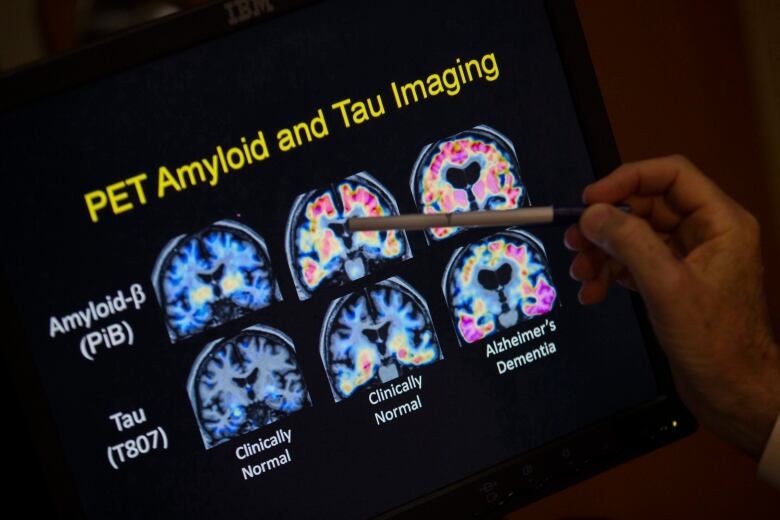
Alzheimer’s is thought to start when a sticky, misfit protein called beta-amyloid leads to brain-clogging plaques and tangles associated with killing off neurons.
The hope is to prevent amyloid from building up in the brain years before symptoms appear.
But so far, the only way to confirm that beta-amyloid has built up is with brain scans that are expensive and hard to get or spinal taps that are invasive and uncomfortable.
That’s where blood screening tests could play a role.
In this week’s online issue of the journal JAMA, Dr. Oskar Hansson, a professor of clinical memory research at Lund University in Sweden, and his team report that a combination of blood tests for specific forms of beta-amyloid and tau proteins correctly identified whether 1,213 Swedish participants, with an average age of 74 and memory problems, in fact had Alzheimer’s about 90 per cent of the time.
“We see this as a major step towards global clinical implementation of an Alzheimer’s blood test,” Hansson said in a release from the Alzheimer’s Association, which partly funded the research.
The experiment needs to be repeated to see how the test fares in more diverse populations, the researchers stressed.
In comparison, dementia specialists using standard methods not including PET scans or spinal taps were accurate 73 per cent of the time, and primary care doctors were correct 61 per cent of the time for the 500 participants who went to those general clinics, the researchers reported.
Initially, about 300 participants in each group were given the blood tests, and then the results were compared to spinal taps and PET scans as well as cognitive tests.
In the United States, labs have started selling a variety of tests to detect signs of Alzheimer’s in blood, but they aren’t widely used since doctors have little to guide them on when to use them. None are formally approved for use by the U.S. Food and Drug Administration or by Health Canada.
High accuracy level needed
Dr. Suzanne Schindler, a neurologist at Washington University in St. Louis who was part of the Swedish study, said it can be difficult to tell whether Alzheimer’s or something else is to blame for a patient’s symptoms.
“I have patients not infrequently who I am convinced have Alzheimer’s disease, and I do testing and it’s negative,” she said.
A study from the Alzheimer Society of Canada predicts that the number of people in Canada living with dementia will triple within three decades. We follow one family who have been on this journey for a few years, as they prepare for the transition from home care to long-term care.
Schindler, who helped lead a comparison of blood tests, said the Swedish one measures a form of tau that correlates with how much plaque buildup someone has. A high level signals a strong likelihood a person has Alzheimer’s, while a low level suggests probably not.
Doctors and researchers should only use blood tests proven to have a greater than 90 per cent accuracy rate, said Alzheimer’s Association chief science officer Maria Carrillo.
Future studies also need to evaluate how the blood tests could be more practical for hospital laboratory workers to conduct instead of outside labs, where the tests can cost more and require highly technical expertise.
It would be unethical to use the blood tests for people who don’t have symptoms but worry about Alzheimer’s in the family except as part of research studies, given that there are currently no treatments to prevent the development of the disease.
What’s more, Alzheimer’s disease may not cause symptoms like memory problems for years. Standard preventive steps include eating a healthy diet and getting enough exercise and sleep.
The findings were also presented on Sunday at the Alzheimer’s Association International Conference in Philadelphia. The maker of an injection used to help diagnose Alzheimer’s disease also contributed funding.