White Coat Black Art26:30Virtual Cancer Screening Service
A handful of new virtual cancer screening programs in British Columbia are connecting people who don’t have a family doctor with potentially life-saving treatment they may otherwise be missing out on.
“We wanted to start a preventative health system where we could hopefully catch things before they developed,” Dr. Stuart Bax, co-founder of CanScreenBC, told White Coat, Black Art‘s Dr. Brian Goldman.
Patients without a family doctor, he said, often seek treatment at a hospital emergency department or urgent care centre, or at a walk-in clinic for what may turn out to be life-threatening cancers.
The people behind such services as CanScreenBC and CancerScreening.ca — which both launched in early 2023 — hope they can help inform the public about cancer screening available to them that they might not otherwise know about in the face of an increasingly overstressed health-care system.
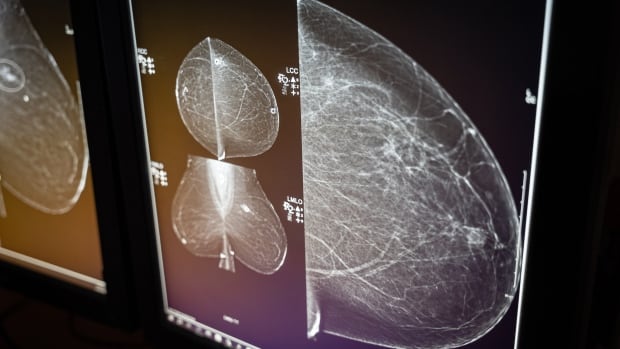
British Columbians can contact these virtual clinics via a video call. There, doctors can provide a client with a referral for tests like mammograms for breast cancer or CT scans for lung cancer, if they’re eligible. Clients can also book a consultation session so they can learn which screening services they’re eligible for in the first place.
Dr. J. Charles Lamb, co-founder of CancerScreening.ca, said people living near the Greater Victoria area can make an in-person clinic visit, though the service is still primarily virtual.

Lamb said he remembers a stark example of a woman who arrived at a hospital emergency department with diarrhea, only for him to find “a rigid mass in her abdomen” that turned out to be metastatic colon cancer.
“I asked her, ‘Have you ever had a FIT test, which is where you test the stool for blood to screen for cancer? Have you ever had a colonoscopy?’ And she said, ‘No, I’ve never been offered one, never knew about it,'” he said.
“It’s totally tragic, because that’s what colon cancer screening is intended to catch as soon as possible.”
Filling need for those without family doctor
According to an April 2023 study by the Canadian Medical Association Journal, an estimated one in five Canadians, or about 6.5 million people, don’t have a family doctor or nurse practitioner they regularly visit.
And a paper published in the journal Preventive Medicine last July found that Ontarians who visited a walk-in clinic because they didn’t have a primary care provider were far less likely to be screened for breast, colorectal and cervical cancer.
CanScreenBC and CancerScreening.ca currently offer screening services for breast, colon and lung cancer. CanScreenBC’s website says it hopes to offer screening for prostate and cervical cancer “in the near future.”
If testing brings up a positive cancer diagnosis, Bax said, his team will continue to support them through the health-care system much in the same way a family doctor would — helping to schedule and co-ordinate future visits with specialists, or sending automated test results, for example.
“We want to be that quarterback. I think the biggest issue facing unattached patients is that lack of accountability and that lack of continuity of care,” Bax said.
‘Simple and straightforward’
Allison Uessman, an English teacher in Vernon, B.C., was connected to breast cancer screening and testing with the help of CanScreenBC, after the two walk-in clinics near her home closed in the past two years.
“I just made an appointment at the clinic and had the mammogram. It was very simple and straightforward. The results were negative in both cases,” she said.
Uessman said she wanted to get checked once she turned 40 and became eligible for breast cancer screening, as her father had colon cancer. She said she felt confident using CanScreenBC because the people running it are doctors themselves.
“[Their website] has their education, where they went to school, their past history. The details like that made me feel confident that they were providing a service that was, you know, covered by B.C. health care,” she said.
Patients’ visits are covered by B.C.’s Medical Services Plan. Bax said he and co-founder Dr. Cal Shapiro are in early discussions with the province about possible longer-term funding for CanScreenBC’s operations.
In a statement to White Coat, Black Art, B.C.’s Health Ministry noted that the government’s 10-year cancer action plan includes improving access to cancer screening. When asked about CanScreenBC’s work, the ministry said: “Any time people can get access to screening quicker is a good thing.”
Primary care provider shortages
B.C. isn’t the only province with programs with the same or similar objectives. In Ontario, the Champlain Regional Cancer Program hired a nurse practitioner to provide and co-ordinate cancer screening for people without family doctors in Ottawa and nearby counties.
Its outreach even included visiting an Amazon warehouse to offer screenings and information to workers there, according to a report in the Globe and Mail.

“We know there is a shortage of primary care providers in British Columbia,” said Dr. Kim Nguyen Chi, executive vice-president and chief medical officer of B.C. Cancer and a medical oncologist at the Vancouver Cancer Centre.
While the B.C. government has “taken steps” to bring in more primary care physicians and nurse practitioners, he said, many people in the province still don’t have a primary care provider or access to one.
“Basically we just need more people … and [the system] really needs those investments to be made.”
Bax said he hopes CanScreenBC and other services like it can help work toward broader, more long-term improvements in the health-care system.
Lamb said he sees a future where virtual cancer screening could be applied nationally, connecting people to tests regardless of which province or territory they live in. That kind of co-ordination could even provide insights by comparing the wait times for tests in different parts of the country.
“We can’t just keep putting Band-Aids on the same old system,” Bax said. “We need to be actually building a whole new system as well — and keeping the current system afloat until that new system comes into place.”
In a Canadian first, the B.C. government has unveiled a new self-screening program for the Human Papillomavirus (HPV), the leading cause of cervical cancer. That will mean many women in the province will be able to avoid uncomfortable Pap smear exams.
