British Columbia is transitioning to test for cervical cancer through HPV screening, meaning patients will be able to provide samples from home and ultimately test less often if their results are negative.
Cervical cancer is a disease in which abnormal cells in the cervix start to grow uncontrollably, forming tumours, according to HealthLink B.C., the province’s online health and wellness resource. A Pap test, or Pap smear, is currently used to detect such abnormal cells.
Approximately 70 per cent of all cervical cancer is caused by the human papillomavirus (HPV), meaning it can be prevented through vaccination and screening.
Leading health organizations believe HPV-based screening is more accurate than Pap tests.
“We hope this will encourage more and more people to get screened,” said B.C. Premier David Eby at a news conference with Health Minister Adrian Dix and other officials, in announcing the transition.
“We know this program is going to save lives.”
Eby said 200 people are diagnosed in B.C. with cervical cancer each year. Currently, screening is recommended every three years for people with a cervix who are between the ages of 25 and 69.
A new report in the Canadian Medical Association Journal recommends self-screening for certain medical issues like cervical cancer to help reduce inequity among certain groups that avoid getting tested. Experts say the measure could help catch more cases of cervical cancer and might potentially eliminate it altogether.
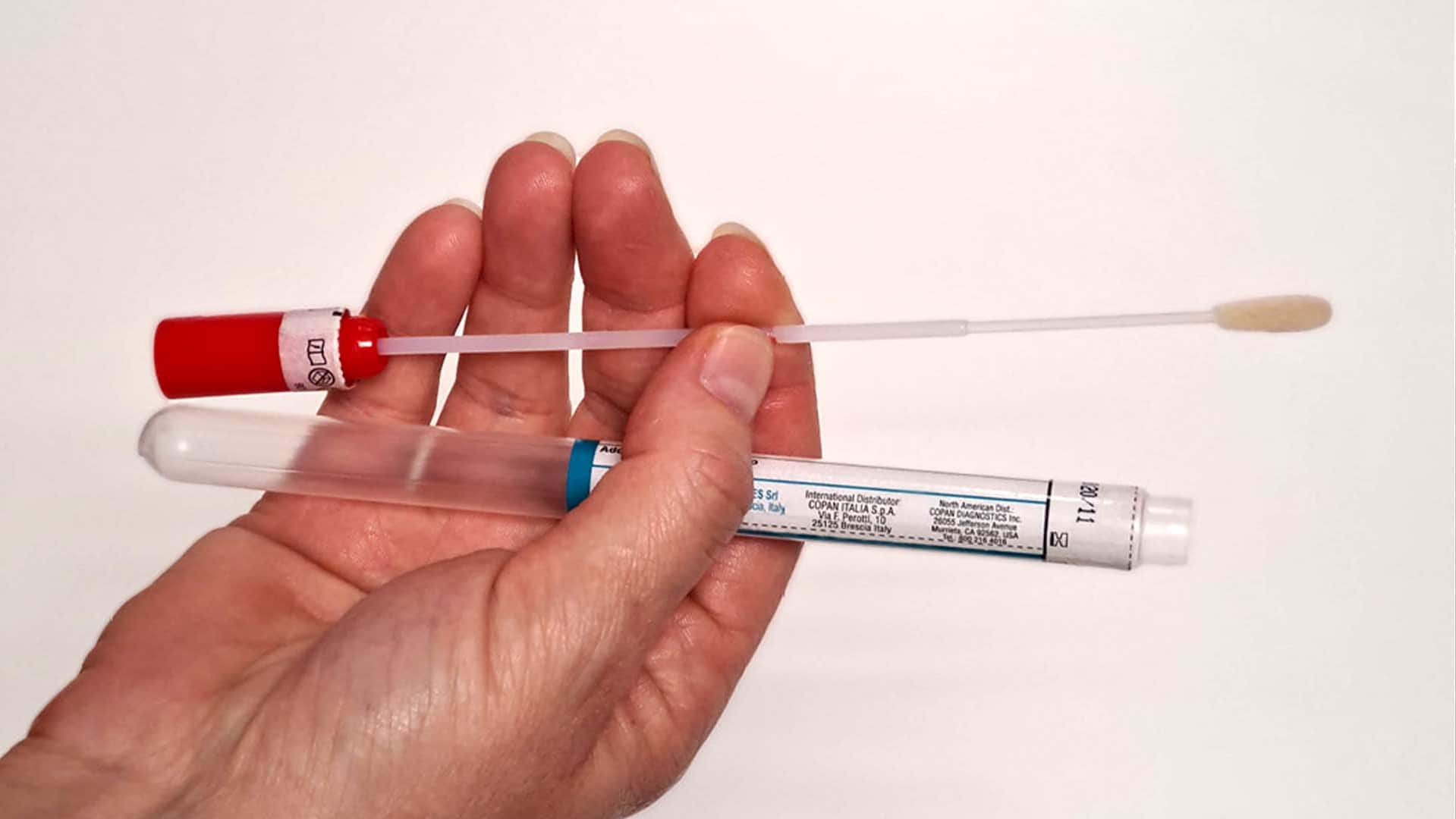
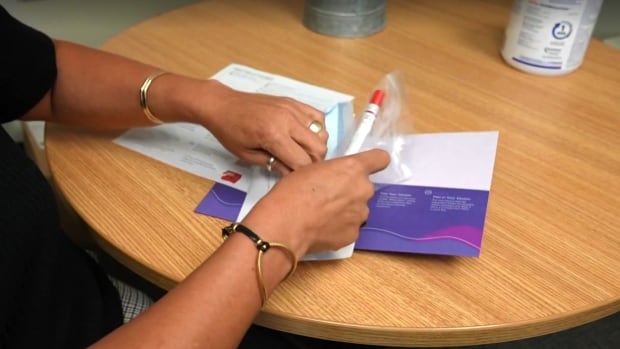
With HPV screening, people will also be able to collect a sample themselves at home, meaning it will be easier for those without a health-care provider to be screened.
A pilot of the HPV-screening program run by the province in 2021 recorded a significant number of people taking part who had never been previously screened or were under-screened, including two-spirit, transgender and gender-diverse people.
Bianca Michell, a First Nations woman who participated in the pilot project by accessing a test kit from Carrier Sekani Family Services in the Central Interior, said she often avoided Pap tests because she did not feel safe or trust health-care providers to do the procedures.
“When I did a Pap test, it was always traumatic and it took a long time for me to recover mentally and emotionally,” she said at the news conference.
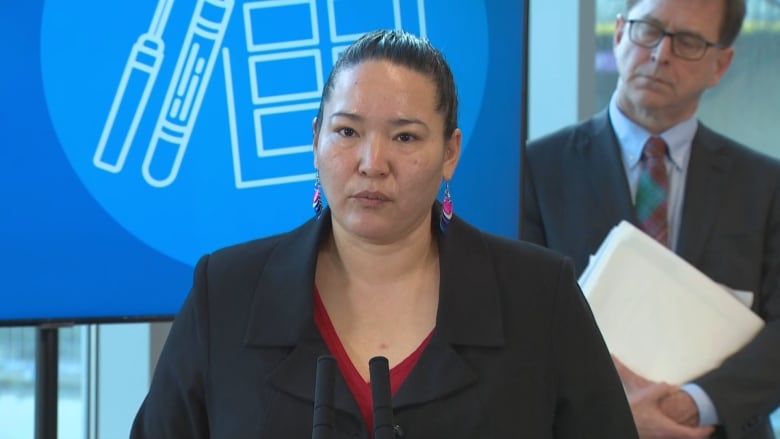
Michell said being able to do the test at home helped her feel safe and ultimately uncovered the need for further health tests.
“This saved my life,” she said, and encouraged others to participate in the new screening plan.
HPV screening will not replace the Pap test in B.C., but patients and providers will be able to choose between them. Patients should continue to seek pelvic exams from health-care providers for other conditions, the province says.
Over time, the province says, HPV screening will increase.
P.E.I. is the only other province in Canada using HPV screening for cervical cancer, B.C. health officials said. B.C. says its the first to offer an at-home screening option.
As of Jan. 29, eligible patients will be able to request free screening kits from B.C. Cancer to complete on their own and then drop off or mail to a lab.
Results will be available in four to six weeks through a health-care provider. People who do not have a health-care provider will be connected with a health clinic to review their results, the province said.
More time between negative tests
HPV screening will allow for less frequent testing — once every five years instead of every three with a Pap test — because the new approach has a “higher sensitivity and higher negative predictive value,” according to materials provided by the province to the media.
The province said randomized controlled trials show HPV-based screening is more effective at identifying those at risk of developing pre-cancerous cervical lesions compared with Pap tests.
HPV is a group of more than 100 different types of related viruses that can spread via intimate skin-to-skin contact during vaginal, oral or anal sexual activity, according to the Canadian Cancer Society.
Infections are very common and while there is no treatment for HPV, most infections will go away on their own, especially in younger people, the society said.
The province said there are about 15 types of high-risk HPV that if not “spontaneously” cleared by the body may cause changes to cells that can lead to cervical cancer over 15 to 20 years.