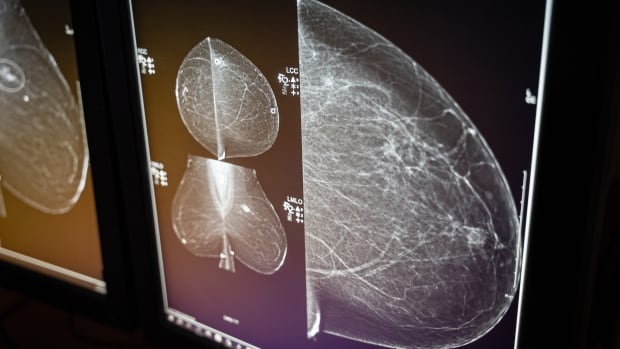
Researchers experimenting with artificial intelligence have found that these tools seem to reliably detect breast cancer, while also reducing a demanding workload for radiologists.
Breast cancer is the most common cancer among adults, with more than 2.3 million cases diagnosed each year, according to the World Health Organization. In most countries, the illness is one of the top two leading causes of cancer deaths in women.
But research shows that early detection and treatment can save lives.
To increase screening capacity and better identify high and low risk breast cancer, two recent studies show that specific applications of artificial intelligence (AI) performed similarly to highly trained radiologists.
“I think that breast imaging, especially mammography, [is] one of the front runners when it comes to the maturity of these AI tools,” said Kristina Lång, lead author on one of the studies.
Lång’s research, which was published in the Lancet Oncology journal last month, is the first of its kind to use AI to detect breast cancer from mammograms in a randomized control trial.
Preliminary results of the Swedish trial show that AI detected more cancer, while keeping false positives to a minimum.
“The results were actually [above] our expectations,” said Lång, a breast radiologist and associate professor at Lund University in Sweden.

Another smaller study, published earlier this week in the journal Radiology, found that radiologists and AI came to similar conclusions after reviewing the same mammograms.
These recent studies are practical examples of the way AI could be used in healthcare to relieve a strained workforce, while ensuring more accurate diagnoses, say experts like Lång.
But other experts warn that the technology is still being refined to ensure it doesn’t over diagnose or miss the cancer.
AI reduced radiologist workload
Radiologists are placing extra significance on Lång’s research as it randomly assigned mammograms from more than 80,000 women to two groups.
One group involved AI-supported screening and the other followed double reading — a standard practice in Europe where two radiologists independently review each mammogram.
In the AI-supported group, the software triaged the scans by determining which ones were of low risk and needed only one radiologist to look at them, or high risk, requiring two radiologists.
Results found that the AI-supported screening group detected about 20 per cent more cancers. It also had a similar number of false positives and women recalled for further analysis as the standard group.
Due to the triaging, the radiologists in the AI-supported screening group read about 44 per cent fewer mammograms than those in the standard group.
“It’s a difficult task to read large volumes of screening examinations in order to detect these small subtle cancers,” said Lång. “You have to be alert.”
Additionally, she said radiology is experiencing a significant worker shortage, so these results show the value of AI in areas with limited staff.
AI can over diagnose, have trouble with dense breasts
“We should be embracing this technology as a really helpful tool to do better and try and diagnose more cancers at an early stage,” said Jean Seely, who heads the breast imaging section at the Ottawa Hospital.
But she said there are still some issues that need to be refined.

In particular, Lång’s study found that AI can over diagnose cancers that might not end up being harmful to the patient.
“We want to call only those patients that really have cancer, but there’s a fine line that we have to balance,” said Seely, who is also a radiology professor at the University of Ottawa.
She also said that, at this point, AI doesn’t compare the current mammogram it’s reading to past ones, nor does it know that the patient might have already had a biopsy for a certain abnormality.
“So to rely on the AI only is really impossible,” said Seely, adding that radiologists are also legally responsible for the mammogram interpretation.
“You have to have a trained person, radiologist, to be able to read those cases and say, ‘yeah this is an appropriate recall, but this is not.'”
Dr. Mojola Omole, a breast oncologist and surgeon in Ontario’s Scarborough Health Network, also thinks AI shows promise for the future, but she’s concerned with the technology’s ability to detect breast cancer in women with more dense tissue.

Typically, she said, Black and Asian women can have more dense breast tissue, which hides the cancer.
“What I worry about sometimes, when we talk about AI medicine, is that populations such as racialized people, when it comes to breast cancer, are not necessarily going to be represented in that sample,” she said.
Omole noted that in the Swedish trial, the race and ethnicity of the women wasn’t recorded.
If women of all backgrounds aren’t included in research like this, said Omole, then it might mean that AI could misdiagnose them or miss the cancer completely.
Dr. Martin Yaffe, a professor and senior scientist at Sunnybrook Research Institute in Toronto, said his team is working on AI that can detect breast density and calculate the chances of a hidden cancer.
“We’re stepping carefully to try and avoid doing anything foolish to get this new technology so that it’s ready for prime time and that involves a lot of testing, and testing under a wide variety of circumstances,” he said.
More research needed to determine tool’s success
Unlike in Europe, mammograms aren’t screened by two radiologists in Canada.
As a result, Ottawa-based radiologist Seely said more research is needed to know how AI would work in the Canadian context.
She notes that it shouldn’t “replace a human,” but that it “adds more value.”
And that’s what breast cancer survivor Marilyn Jordan also thinks about it.
“I feel positive about AI facilitating quicker diagnosis and catching more cancers than at the current time,” said the 68-year-old Vancouver resident.
Jordan completed her breast cancer treatment last September after she pushed to get a mammogram a year before her regularly scheduled screening appointment.
Even though AI can over diagnose, Jordan said she’d rather the tool be “extra cautious” and catch everything.
“Maybe it’ll find a cyst that needs to be monitored annually, ” she said.
The Swedish trial is still ongoing and looks to better evaluate AI-supported screening by finding out whether it reduces the rate of interval cancer.
Interval cancer is when a person is diagnosed with cancer after a normal result and before their next screening appointment.
The interval cancer rate will be determined after the participants have a follow-up two years from their screening in December 2024.
Lång said they’re also interested to know whether the use of AI is cost effective.
“I think the synergistic effect, when humans work together with this AI tool, to use them in a safe and smart way, we can really … improve both the efficiency and the quality of healthcare.”





