Health insurance costs are set to climb at their steepest rate in a decade as prices are pushed up by higher labor costs and growing demand for weight loss drugs like Ozempic.
The cost of employer-funded health insurance coverage will rise by 6.5 percent next year, according to figures obtained by the Wall Street Journal from consulting firms Mercer and Willis Towers Watson (WTW).
Already companies pay on average $14,600 a year per employee – making it one of the biggest expenses for US companies.
Separate estimates from health research non-profit KFF suggest premiums for plans sold under the Affordable Care Act will also rise by 6 percent, reports the WSJ.
Hospitals are struggling under the weight of higher labor costs – thanks to rising nurse salaries – as well as demand for expensive diabetes and obesity drugs.
Hospitals are struggling under the weight of higher labor costs – thanks to rising nurse salaries – and demand for expensive diabetes and obesity drugs
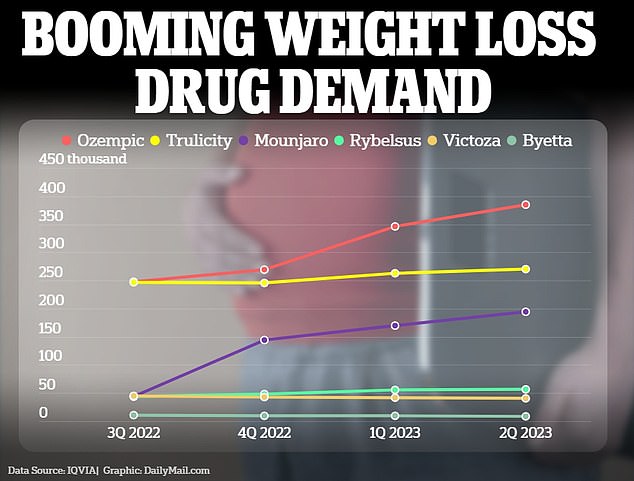
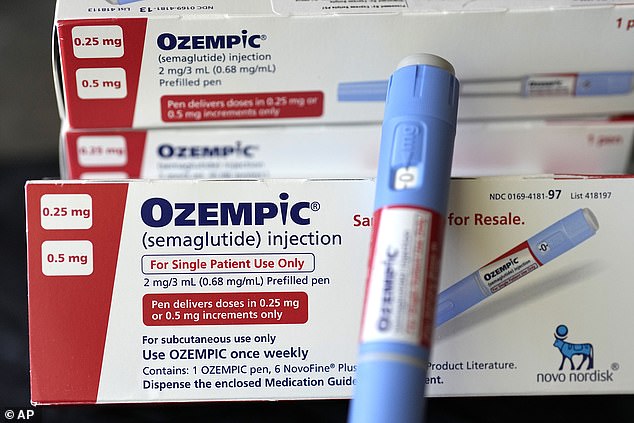
Ozempic and its sister drug Wegovy have experienced a surge in popularity over the last year and has been linked to a host of celebrities including Amy Schumer and Sharon Osbourne. A new competitor – Mounjaro – was also approved by the FDA last year.
But such drugs – which are injectable semaglutide designed to lower blood sugar levels – can cost hundreds of dollars a month.
Wegovy lists for more than $1,300 for a 28-day supply while Ozempic is around $900 a month.
WTW previously estimated that a typical employer’s drug spending could increase by 50 percent if half of the employees who were eligible for Wegovy took it.
Their popularity has resulted in a pushback from employers who are cautious about covering the medicine on their plans.
Fewer than 25 percent of companies will cover a drug specifically for the purpose of losing weight, according to a survey by the International Foundation of Employee Benefit plans.
Those that do tend to be bigger firms with more than 5,000 staff members.
Jennifer Chang, knowledge adviser at the Society for Human Resource Management, previously told the WSJ: ‘We certainly are kind of at the beginning of the curve in terms of how insurance companies and healthcare plans are going to tackle this.’
Despite this, Debbie Ashford, from health benefits consultant and brokerage Aon, warned ‘utilization is skyrocketing.’
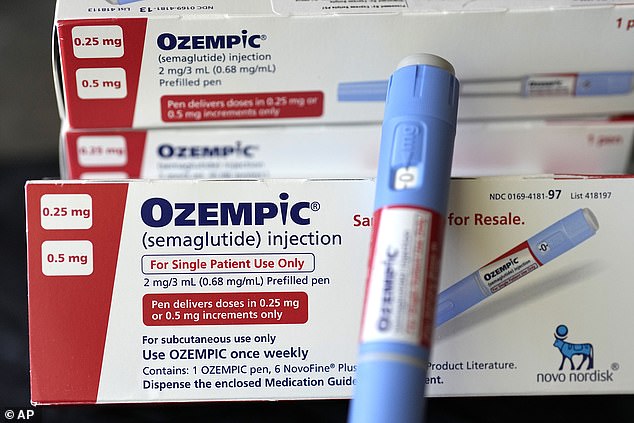
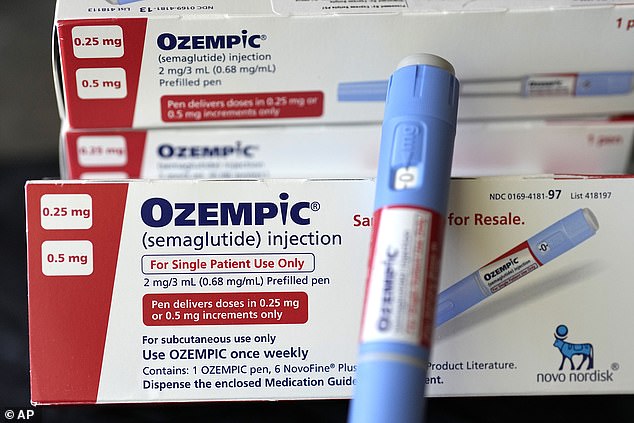
Ozempic and its sister drug Wegovy have experienced a surge in popularity over the last year and has been linked to a host of celebrities including Amy Schumer and Sharon Osbourne.
The increase in premiums marks a stark reversal from years of slow increases to health insurance costs, thanks to stalling doctor and hospital visits during the pandemic.
The issue is compounded by higher labor costs: the average salary for a registered nurse grew by 4 percent in 2021 following the pandemic. Last year the median pay of a registered nurse wads $81,220, according to figures from the Bureau of Labor Statistics.
Hospitals are now winning price increases from insurers which create a domino effect unto employers.
WTW chief actuary Tim Stawicki told the WSJ: ‘Inflation we saw a year ago is finally making its way into the contracts. It’s like a delayed reaction.’
The firm surveyed more than 450 US employers between June and July, finding plans would on average increase by 6.4 percent. It makes it the biggest increase since 2012.
Companies will have to decide whether to take the hit out-of-pocket or increase the contributions they take from workers’s paychecks for the coverage.
The majority of workers will learn about their work healthcare plans for 2023 in the annual fall enrollment period.
Source: | This article originally belongs to Dailymail.co.uk