
Patients going to A&E because they were having a mental crisis had to wait three weeks for a bed at one of England’s busiest hospitals, it has been revealed.
The patients had to stay in a short stay area with no natural light at Royal Sussex County Hospital in Brighton because of a shortage of mental health beds.
A Government inspection dated April 26 to 27 found the patients stayed in the side rooms for an average of 52 hours before being admitted to a ward.
But some had to stay in the area — which had no TV or radio and only had a toilet and basin available — for two to three weeks.
The NHS says patients in a mental health crisis ‘might think about suicide’ or ‘experience hallucinations and hear voices’.
It comes amid a crisis in NHS A&E departments, with dozens of A&E patients with physical problems forced to wait two days for a bed at one of England’s busiest hospitals.
A shocking 865 people waited longer than a day to be admitted after showing up at Royal Cornwall Hospitals Trust’s emergency departments in April and May.
Of them, 89 endured waits of at least 48 hours for a bed during the same time period.
And last weekend, a sign put up in A&E at Royal Bolton Hospital, run by Bolton NHS Foundation Trust, warned of waits of ’40+ hours for a bed’.
The NHS is currently battling its busiest summer on record with pandemic backlogs, rising Covid staff absences and ongoing handover delays.
Emergency wait times have hit record levels across England, with latest data showing 12-hour waits are increasingly becoming more regular.

Mental health patients have been forced to wait up to three weeks in an emergency department at Royal Sussex County Hospital in Brighton, a Care Quality Commission has revealed




Some 89 patients were left stranded waiting for a bed for more than 48 hours in A&Es run by Royal Cornwall Hospitals Trust in April and May. Pictured Bodmin Hospital, which is run by the trust
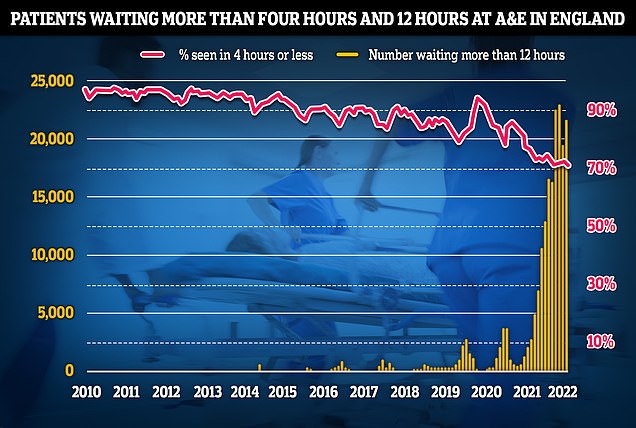
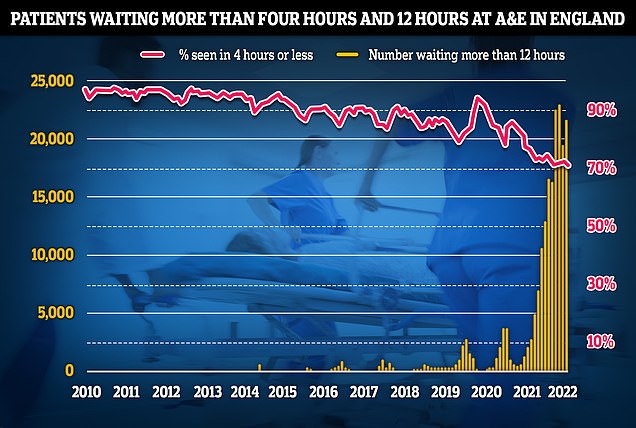
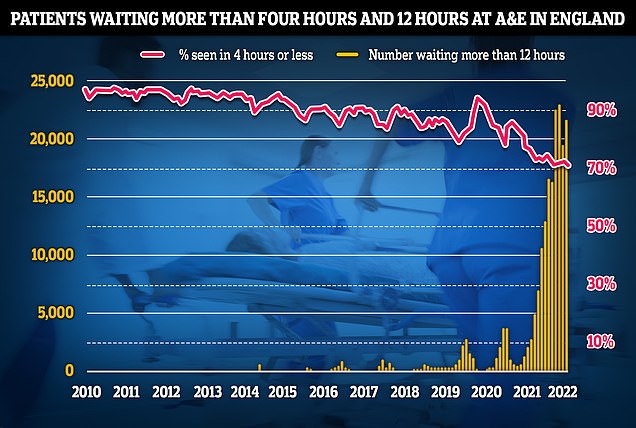
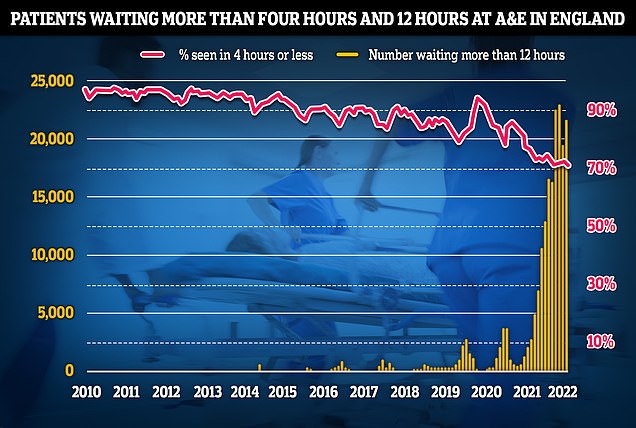
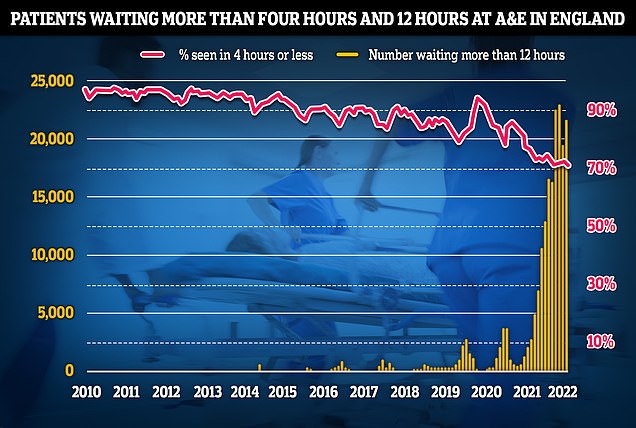
Some 22,034 people had to wait more than 12 hours in A&E departments in England in June from a decision to admit to actually being admitted, NHS England said. The figure is up from 19,053 the previous month, but still below a record of 24,138 in April, which was the highest for any calendar month in records going back to August 2010
More than 22,000 Britons queued for more than half a day in emergency departments before being seen last month. The target is four hours.
A Care Quality Commission — a public body that rates health and social services in England — report into Royal Sussex County Hospital rated its urgent and emergency services as requiring improvement.
Mental health patients at the hospital, run by University Hospitals Sussex NHS Foundation Trust, only had access to a shower in a neighbouring ward while waiting for beds.
They were checked by mental health liaison teams each day.
University Hospitals Sussex NHS Foundation Trust chief executive George Findlay said: ‘Since I returned to the trust two months ago, I have been extremely impressed by the efforts and commitment of colleagues in all our hospitals to always provide the highest standards of patient care despite the pressures on our services.
‘I am pleased, therefore, that the inspectors recognised a real commitment to patient care across all services and noted the wide range of improvements made since their previous inspection of maternity and surgery in September 2021.
He added: ‘We recognise there is more work to do and we are doing it.
‘We are successfully recruiting new people to our teams and filling our staffing gaps.
‘We have secured investment and are finalising a business case to improve the layout and functionality of the emergency department at the RSCH and are continuing to build on the improvements we have made in all areas.
‘Some issues take longer to resolve than others, but I want people across Sussex to know that when they come to a UHSussex hospital, we will do all we can to provide the safe, high quality, effective care they expect.’
Meanwhile, latest data for the Royal Cornwall Hospitals Trust shows at least one patient with physical ailments a day waited more than 48 hours to be admitted after going to A&E in April and May.
The trust has admitted some of the patients were stranded in corridors or waiting rooms ‘on rare occasions’ but ‘they are always moved as quickly as possible to another area’.
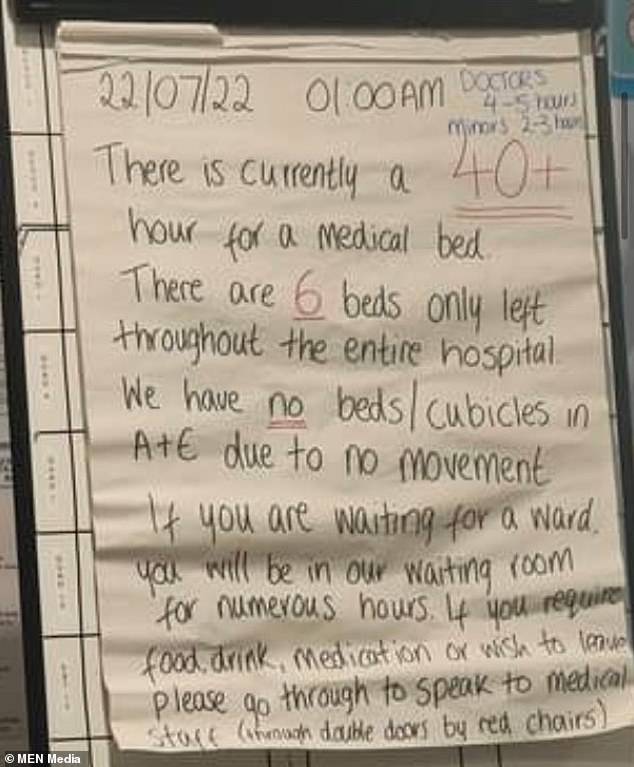
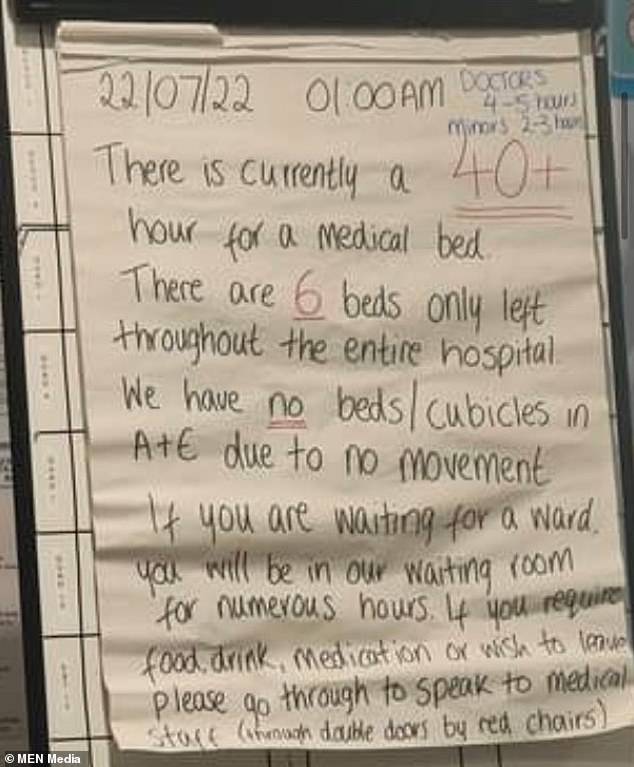
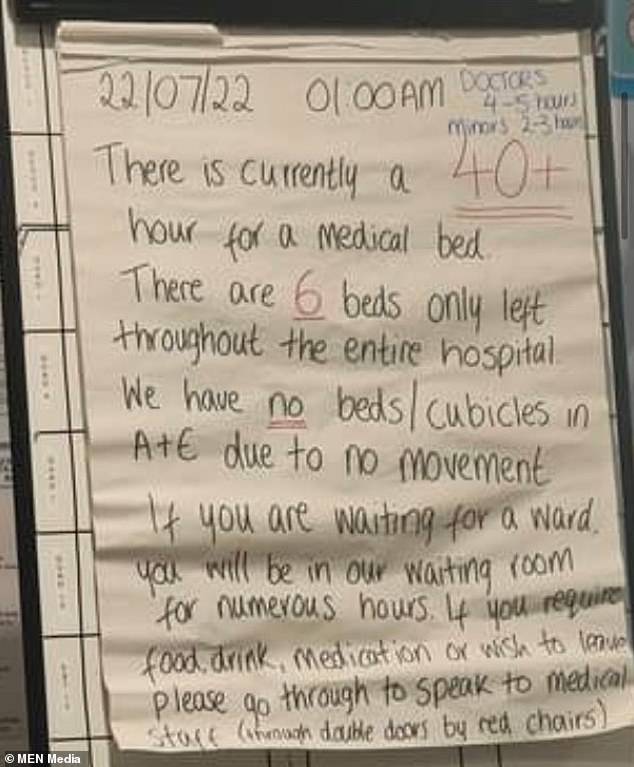
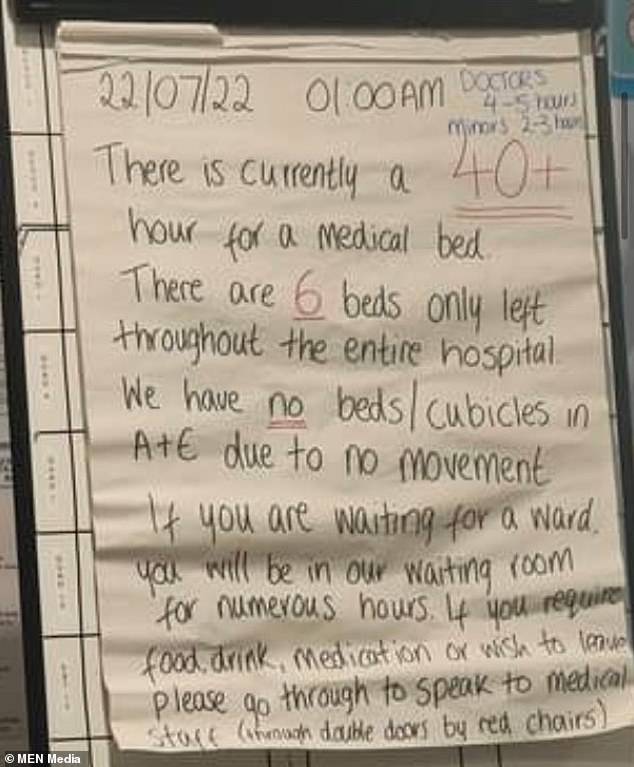
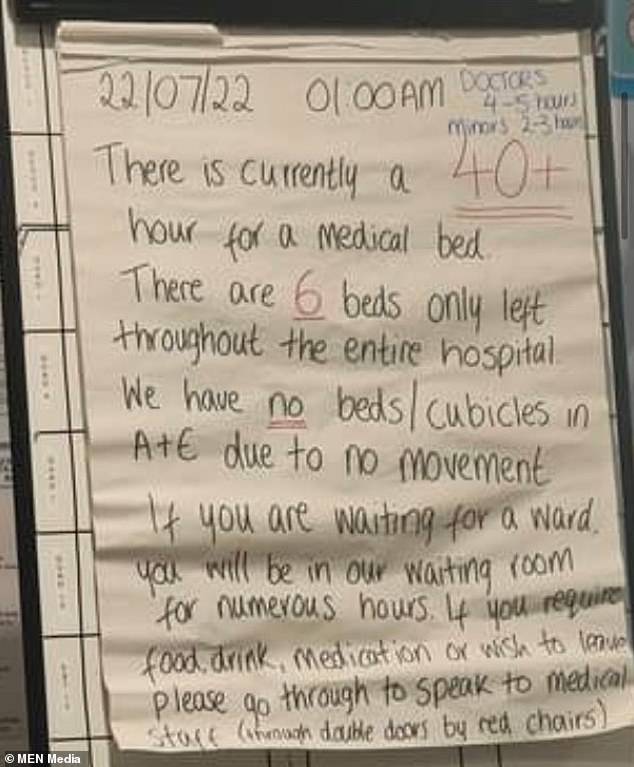
The NHS is currently battling its busiest summer on record with patients told they could wait 40 hours before being admitted to Royal Bolton Hospital in Greater Manchester last week (pictured)
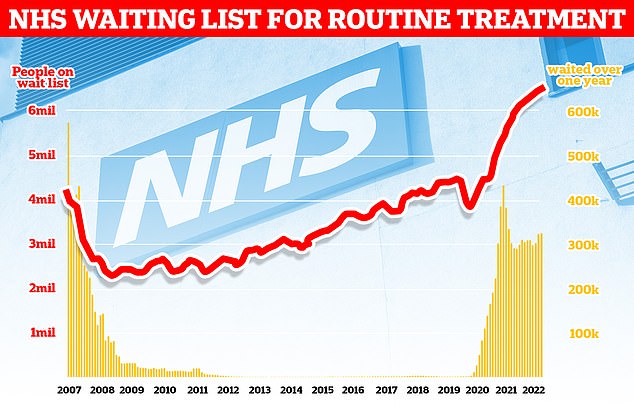
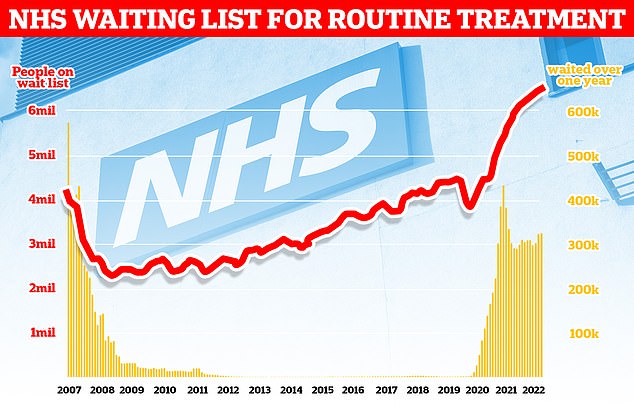
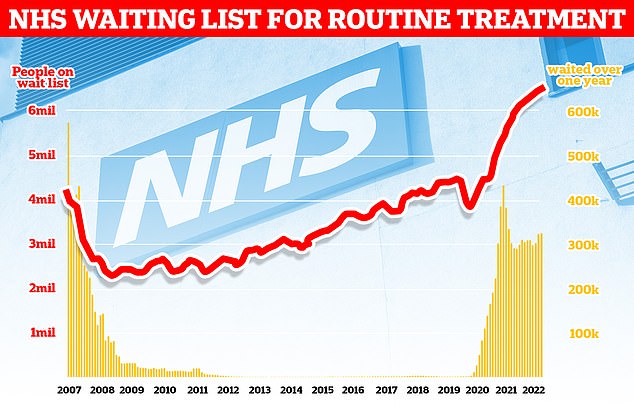
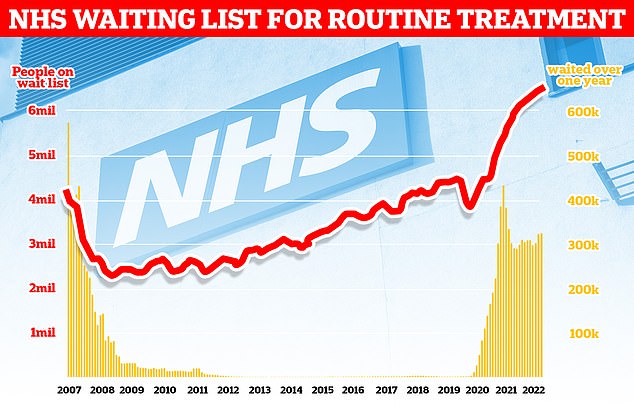
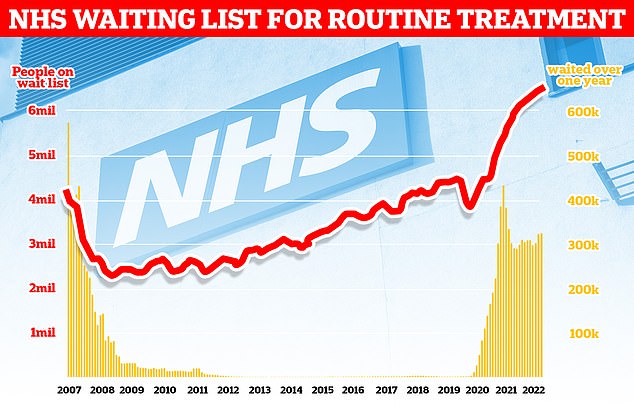
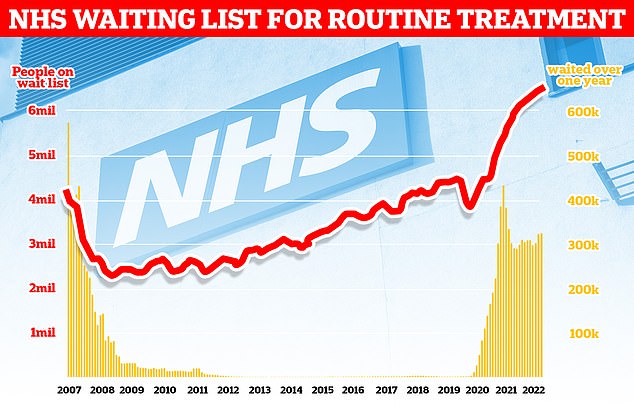
The NHS backlog for routine treatment grew from 6.4million to 6.6million in May, the latest month with data, meaning one in eight people in England are now waiting for elective care, often in pain
In most cases, they were kept in ambulance handover areas, minor treatment areas, A&E cubicles and rapid assessment units, according to hospital bosses.
It is unclear how widespread the astonishing waits have become elsewhere because trusts do not routinely publish A&E admission times over 24 hours.
The waits happened despite A&Es in the area seeing half of the admissions they had in the same time period in 2019 before the pandemic.
No patient waited longer than 12 hours in those months pre-pandemic, compared to 607 in June, according to the most recent data.
Bed-blockers — patients ready for discharge who are unable to leave — are part of the problem, according to the trust.
Many hospitals are also suffering with less staff than they had pre-pandemic, with staff absences also increasing because of Covid infections.
National data indicates there has been no improvement in wait times in recent months, with emergency 12-hour waits in June higher than in May.
Trust bosses in Cornwall have also also warned demand will increase in the coming weeks, as the county welcomes millions of tourists over summer.
Those who faced the longest waits at the trust were placed in corridors ‘only on rare occasions, and they are always moved as quickly as possible to another area in the department,’ a spokesperson for the trust said.
They told the HSJ: ‘Within our hospitals we have opened as many extra beds as possible.
‘We are reducing admissions by reviewing lower acuity patients on arrival and during their inpatient stay to maximise the use of alternative settings and services, wherever appropriate.
‘This is not a problem our hospitals can solve alone, and we continue to work together with our system partners to tackle the capacity gaps in the care home and domiciliary care sectors, which are largely driven by the high level of staff vacancies.’
There is increasing concern about how the NHS A&E system is coping over what some are calling it’s worst ever summer as it battles a fresh surge of Covid, hot weather and a wave of staff absences – on top of pandemic backlogs.
Heart attack patients waited more than 50 minutes for an ambulance on average in England last month — nearly triple the NHS target — and more than 22,000 Britons queued for 12-plus hours in A&E before being seen.
Callouts to the most urgent cases have also risen by a third in recent months, with the average patient with a life-threatening emergency now waiting nine minutes for paramedics, compared to the seven-minute goal.
The health service’s monthly performance stats lay bare the crisis in emergency departments as medics wrestle with increasing Covid hospital and staff sickness rates, excess admissions caused by the heatwave and pandemic backlogs.
Meanwhile, the number of people in England waiting to start routine hospital treatment has also risen to a new record high. A total of 6.6million people were waiting to start treatment at the end of May.
This is up from 6.5million in April and is the highest number since records began in August 2007.
England’s GP crisis deepens: Staff numbers fall to lowest level on record, fewer than HALF of consults are with a qualified doctor and up to one in five appointments last just five MINUTES
The number of qualified GPs has dropped to its lowest level on record and just one in four family doctors work full time, according to official data that highlights the ‘catastrophic’ crisis in general practice.
There were around 27,500 fully-qualified, permanent family doctors working for NHS England last month, down from about 28,000 in June 2021 and 1,500 fewer than five years ago.
The figure comes despite Boris Johnson‘s 2019 manifesto pledge to increase GP numbers by 6,000 by 2024. Ministers have since admitted that target will not be met.
Health bosses have warned the crippling workforce shortages, combined with unprecedented demand for a GP following the pandemic, has created an untenable situation that threatens patient safety.
Meanwhile, just 23 per cent of permanent NHS GPs work 37.5 hours or more a week, a drop from one third in five years. It follows research showing most family doctors now only work three days or less a week.
Patients have struggled to secure appointments or see a doctor face-to-face, which has seen some desperate people resort to turning up at A&E.
Separate figures suggest other NHS staff are increasingly picking up the burden as GPs wrestle staffing problems.
Data for June shows fewer than half of all appointments were carried out by qualified doctors. The rest were seen by other staff, including nurses, physiotherapists and even acupuncturists.
Nearly one in five appointments nationally lasted five or fewer minutes last month, in what campaign groups said was a sign GP surgeries have turned into ‘revolving door’ practices in an effort to get patients in and out as fast possible to get through huge workloads.
Appointments are meant to last no less than 10 minutes according to NHS best practice, while unions have pushed to increase the time to 15 minutes to ensure ‘quality of care’.
Meanwhile, around 65 per cent of appointments were made face-to-face during the month, down from nearly 80 per cent before the pandemic.
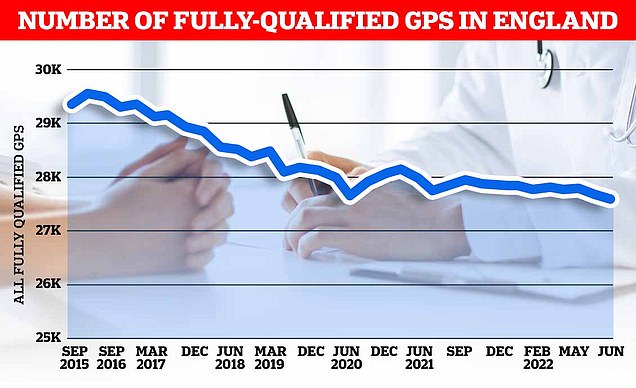
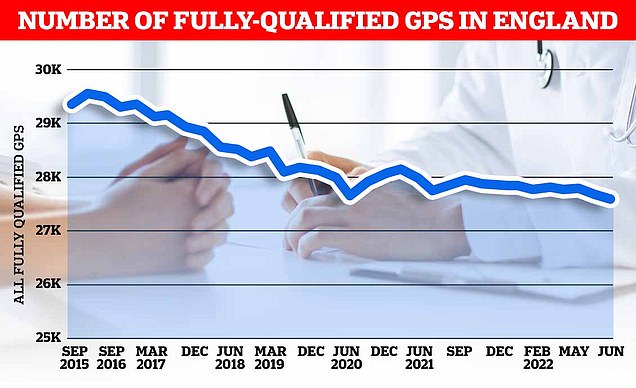
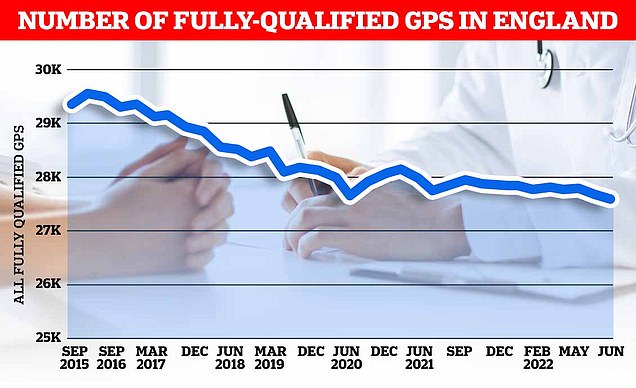
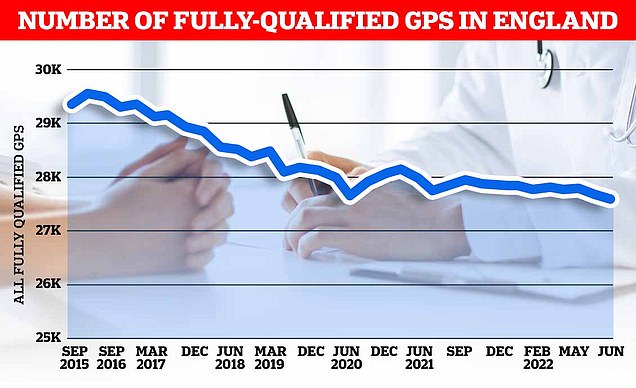
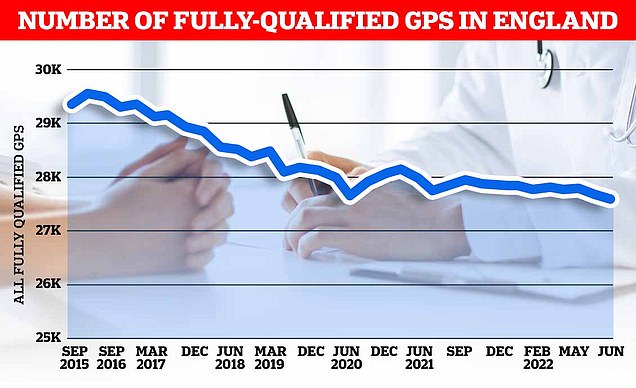
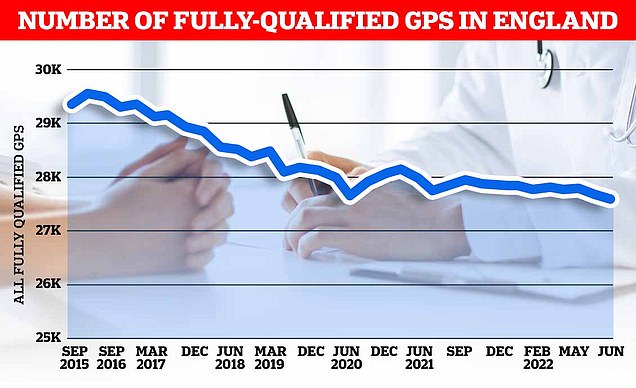
There were just 27,558 full-time equivalent, fully-qualified GPs working in England last month, down 1.6 per cent on the 18,000 recorded in June 2021. It was down 5.3 per cent on the more than 29,000 working in June 2017
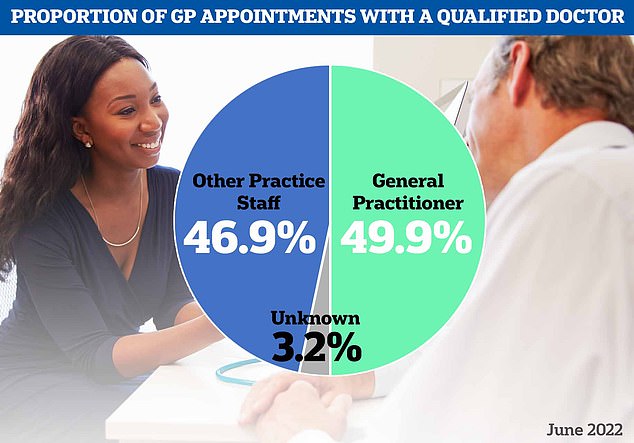
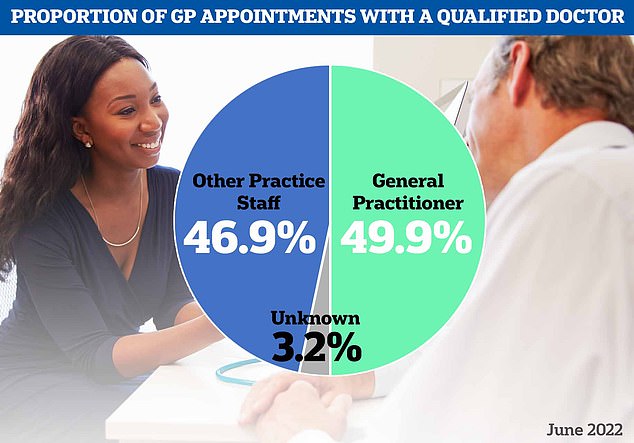
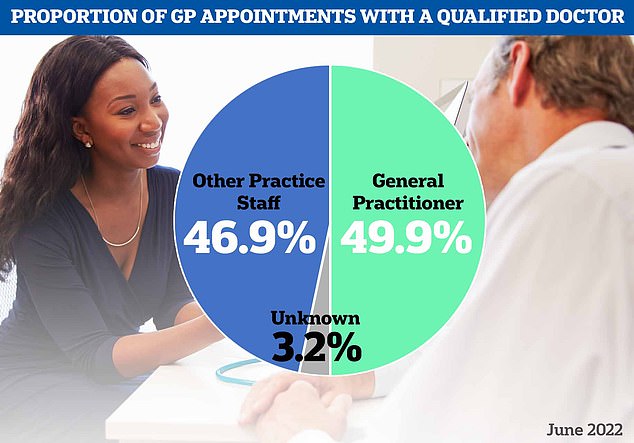
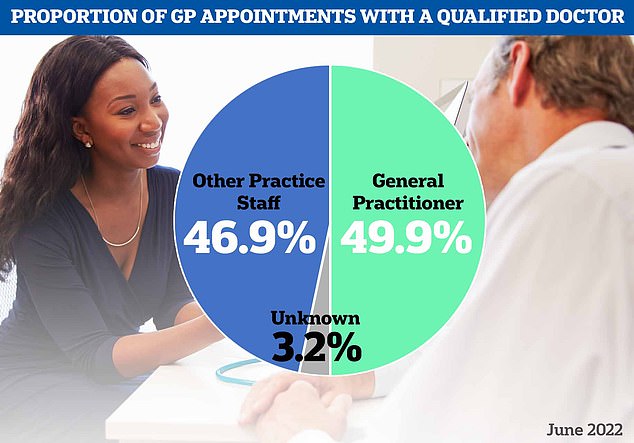
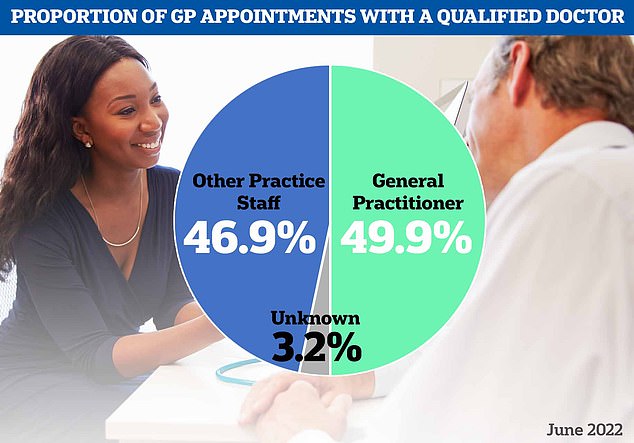
Meanwhile, separate figures today showed less than half of all appointments made last month saw patients seen by qualified doctors. Nearly 47 per cent of patients were seen by nurses or other staff, which can include acupuncturists and physiotherapists
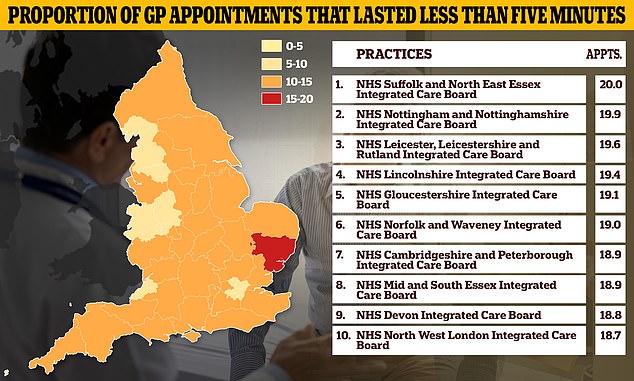
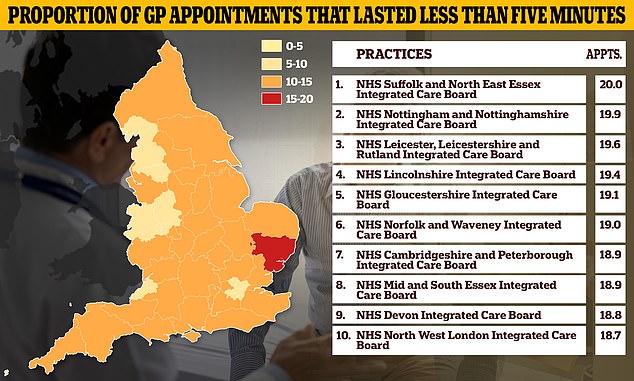
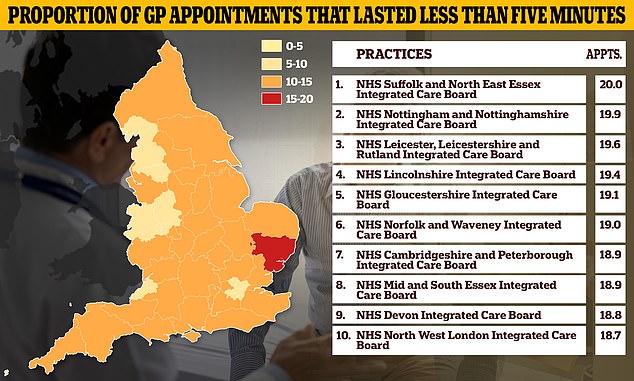
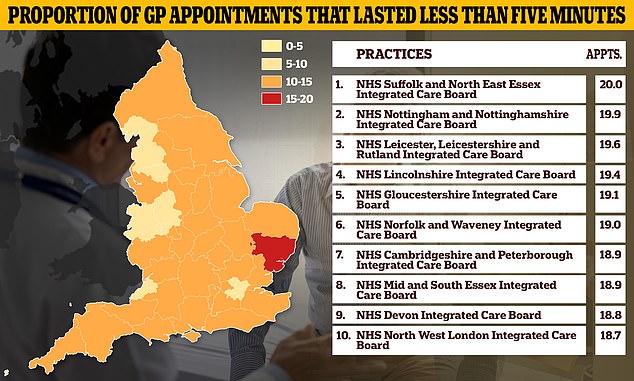
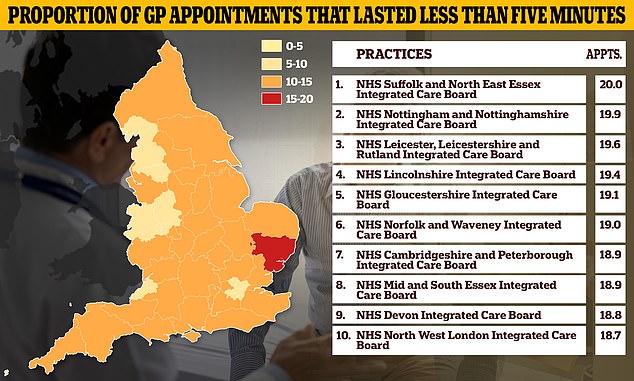
One in six appointments in the country lasted up to just five minutes last month, with even higher proportions seen in some areas of the country. NHS Suffolk and North East Essex Integrated Care Board saw 20 per cent of patients in five minutes or less
Increasing numbers of doctors are reducing their working hours and retiring early, while some are leaving to the private sector or abroad because of the huge increases in pressure put on them.
The NHS Digital data shows the number of full-time equivalent GPs that are fully qualified have dropped to its lowest level since records began in September 2015.
All figures are based on the number of full-time equivalent posts in the GP workforce, and do not include trainees or locums.
Emily Jones, director of risk and healthcare at consultancy firm Broadstone, said: ‘The declining number of qualified GPs in the UK is pushing the NHS to breaking point as demand continues to rise amid a growing backlog.
‘The crisis risks a vicious spiral as more GPs quit the practice due to the intensifying workload heaping further pressure on those that remain in service.
‘Patients are now waiting longer than ever for appointments with their GP for new diagnoses as well as ongoing treatments for existing conditions like cancer and diabetes.
‘This is having a catastrophic impact as life threatening illnesses are being left undiagnosed until it is sadly too late for effective treatment.’
Meanwhile, the proportion of GPs working part-time between – 15 and 37.5 hours a week – has climbed from around six in 10 (62 per cent) to seven in 10 (69 per cent), according to figures for June.
GPs said doctors have been forced to drop their working time to avoid burnout because of the ‘unsustainable’ pressures being put on them by ever-increasing demand.
Professor Martin Marshall, chair of the Royal College of GP, told MailOnline: ‘Despite repeated promises to boost GP numbers, today’s figures show that we have more than 1,500 fewer qualified, full-time equivalent GPs than we did five years ago.
‘The result is a chronically over-stretched and under-resourced general practice service, with GPs and their teams working to their absolute limits to deliver increasingly complex care to the ever-rising number of patients that need it.
‘This is reflected in today’s GP consultation figures, which show general practice is continuing to deliver more consultations every month than pre-pandemic, with more than 26million appointments delivered in June, and over 44 per cent of those on the same day they were booked.’
He added: ‘Working at this intensity is unsustainable and it’s unsafe for both patients and staff. An exhausted GP is not able to practice safely or deliver the high-quality care and services they are trained and want to deliver for patients.
‘This is leading to GPs and other members of our teams burning out and having to evaluate their futures working in general practice, in some cases leaving the profession earlier than planned and in others reducing contracted working hours to make the job more sustainable.
‘Yet working “part time” in general practice often means working what would normally be considered full-time, or longer — and will likely include many hours of paperwork on top of patient appointments.’
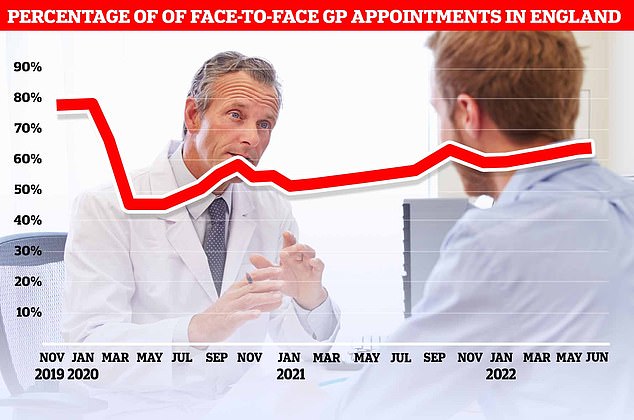
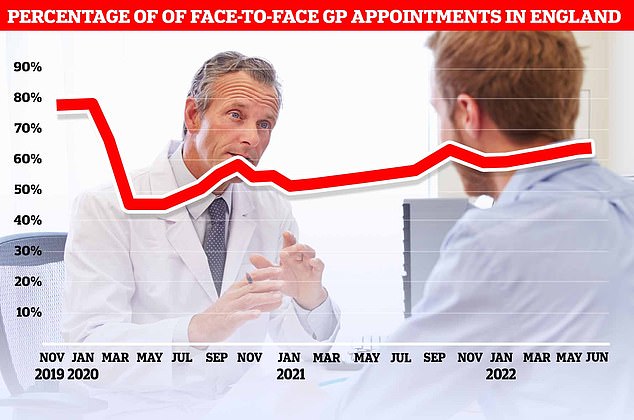
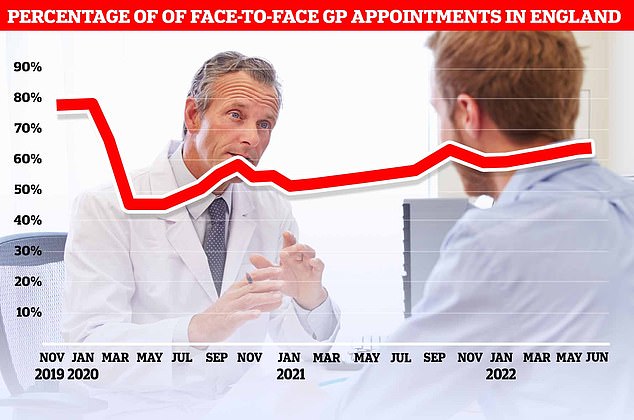
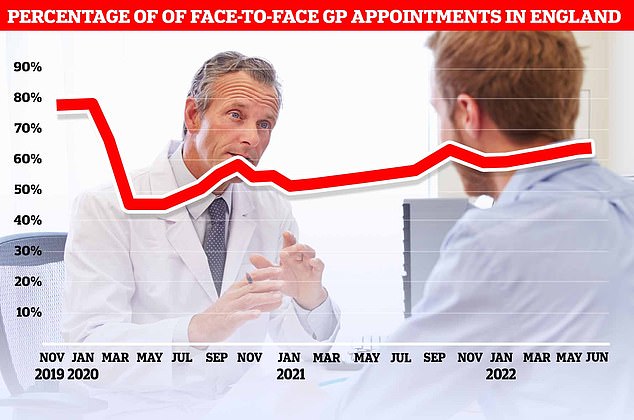
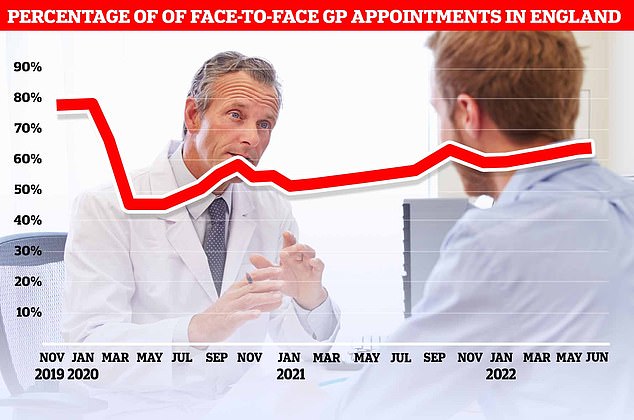
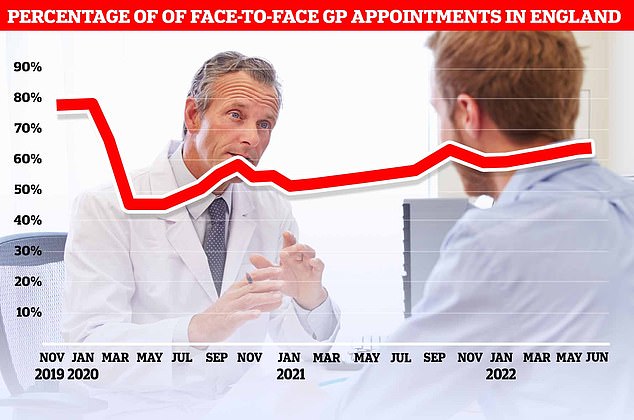
The proportion of GP appointments that were face-to-face rose slightly to 64.8 per cent last month, up from 64.1 per cent in May
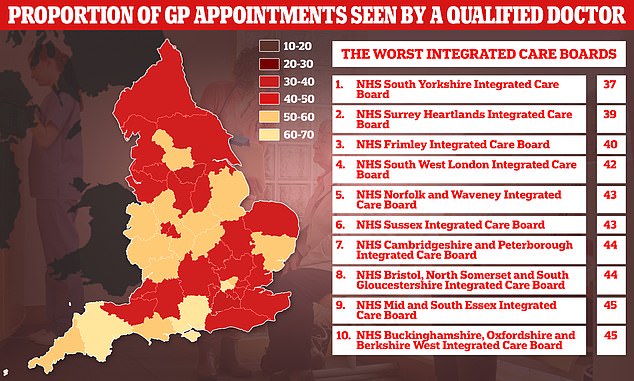
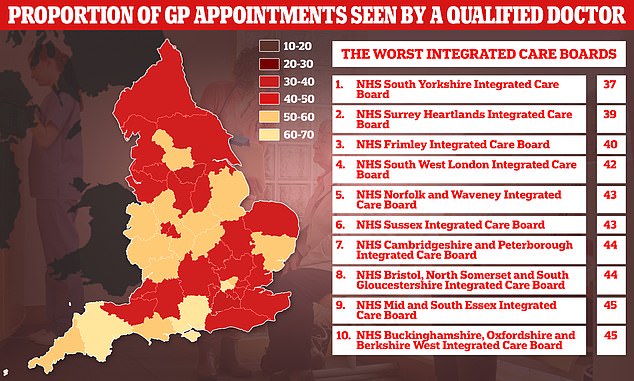
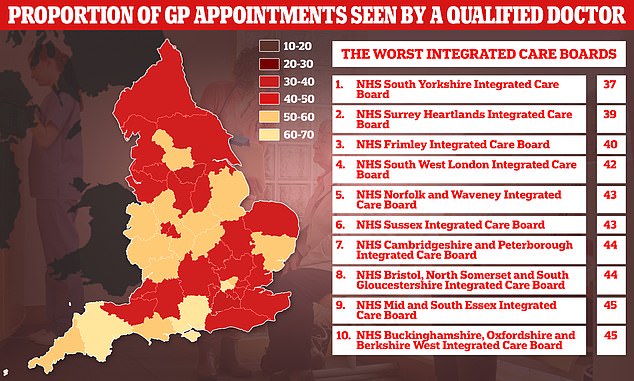
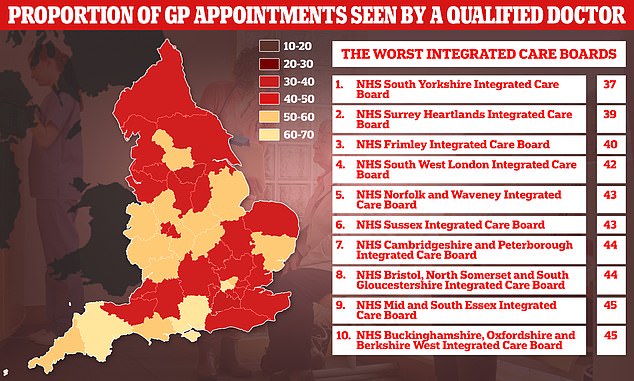
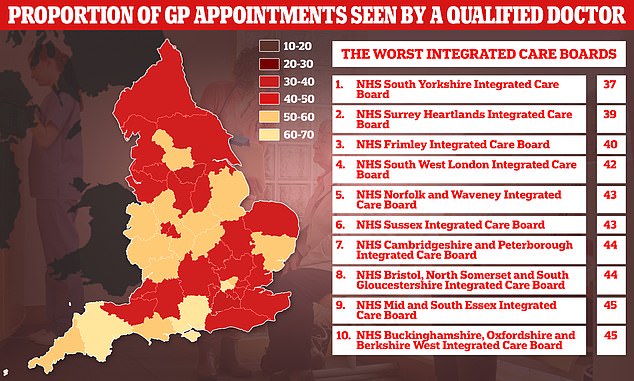
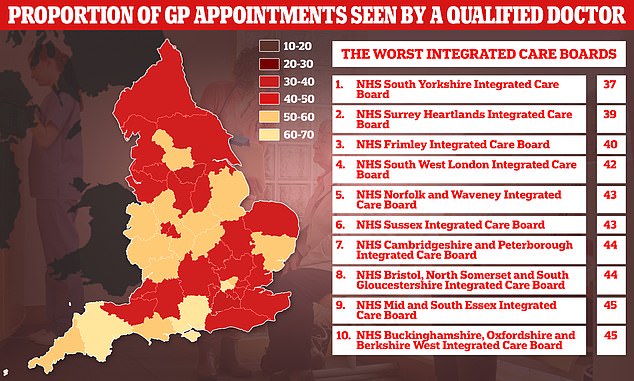
Graph shows: The proportion of patients seen by a fully qualified doctor at GP appointments in different regions of England in June
Separate data from NHS Digital shows the proportion of appointments where patients are seen by qualified doctors fell to just 49.9 per cent last month, down from 50.2 per cent in May.
The figures are calculated based on the number of sessions with a GP in attendance as a proportion of all appointments, which include some appointments where the type of healthcare professional was not recorded.
This means there may have been slightly more appointments that were attended by GPs than are reflected in the data.
One in six appointments in the country lasted up to just five minutes last month, with even higher proportions seen in some areas of the country.
NHS Suffolk and North East Essex Integrated Care Board saw 20 per cent of patients in five minutes or less.
The area with the next highest proportion of sub five-minute consultations was NHS Nottingham and Nottinghamshire Integrated Care Board (19.9 per cent)
It was followed by NHS Leicester, Leicestershire and Rutland Integrated Care Board (19.6 per cent), NHS Lincolnshire Integrated Care Board (19.4 per cent) and NHS Gloucestershire Integrated Care Board (19.1 per cent).
Dennis Reed, director of elderly charity Silver Voices, told MailOnline: ‘I find it difficult to comprehend how a GP visit can take less than five minutes. That hardly provides enough time to take your coat off and sit down.
‘Routine and speedy transactions, such as repeat prescriptions or blood pressure checks are now carried out by other practice staff, and it is only complex cases, which are referred for GP attention.
‘These “revolving door” statistics show the pressures that GPs are under and the potential dangers to patient safety from rushed diagnoses.’
The British Medical Association (BMA) — a trade union representing nearly 160,000 doctors — advises all appointments last at least 15 minutes to ensure ‘the quality of care provided, preserve patient satisfaction, and reduce the need for repeated consultation with patients’.
Appointments are supposed to be fixed at 10 minutes according to NHS best practice. More than half (51.8 per cent) of appointments lasted less than 15 minutes, according to the figures.
Meanwhile, the proportion of GP appointments that were face-to-face rose slightly to 64.8 per cent last month, up from 64.1 per cent in May.
The amount of consultations that are made in-person are still below pre-pandemic levels, with concerns raised doctors are less able to spot potentially dangerous diseases over the phone or on Zoom calls.
The data comes after the annual GP Patient Survey earlier this month revealed half of sick patients have not seen their GP in the last year, with most saying it was because they could not get an appointment.
Of patients who had avoided seeing a GP in the past year, more than a quarter (27 per cent) said they found it too difficult to book an appointment — more than double the number in 2021 (11 per cent).
Some 20 per cent were worried about the burden on the NHS, while 12 per cent said it was due to being worried about catching Covid, down from 17 per cent in 2021.
Of those who did manage to see a doctor in the last 12 months, half (49 per cent) said they were not seen as quickly as they wanted, up from 41 per cent.
Just 56 per cent said they had a good experience making an appointment compared to 71 per cent a year ago.
Source: | This article originally belongs to Dailymail.co.uk