

The psychedelic DOI reduces anxiety by targeting specific neurons in the ventral hippocampus, offering a path to new treatments that avoid hallucinatory side effects.
For centuries, indigenous cultures have used psychedelics, with empirical evidence demonstrating their ability to alter mood and perception. In recent years, there has been a resurgence of interest in these substances due to their potential therapeutic benefits for psychiatric conditions like anxiety and depression. Despite this, the underlying mechanisms by which psychedelics influence mood and behavior remain unclear.
A team of researchers led by Prof. Vidita Vaidya from TIFR Mumbai, in collaboration with research groups from Cornell, Columbia, and Yale University mapped the precise part of the brain, and the specific class of neurons within this brain region, that drives the decrease in anxiety caused by acute treatment with the psychedelic DOI.
DOI’s Effects on Anxiety and the Brain
The psychedelic DOI when administered to rats or mice systemically, decreases anxiety behavior on approach-avoidance behavioral tasks, such as the elevated plus maze and open field test. To precisely pinpoint the part of the brain that responds to DOI and drives this decrease in anxiety behavior, local infusions of the drug into targeted brain regions uncovered a critical role of the ventral hippocampus in mediating this effect of the psychedelic DOI.
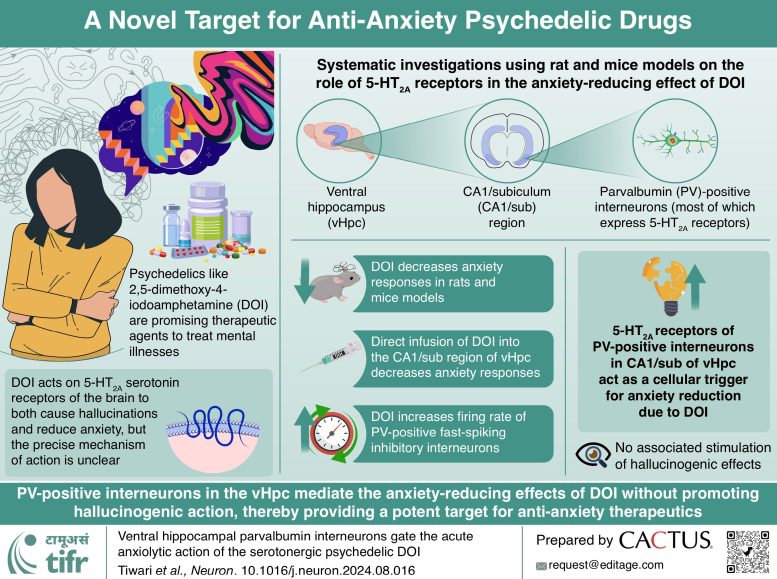
Further, the study uncovered that the psychedelic DOI targets the serotonin2A receptor in the ventral hippocampus to exert its effects on anxiety. At the same time, the team also ruled out contributions from other brain regions including the prefrontal cortex and amygdala.
What was striking is that the ventral hippocampus while vital for the decrease in anxiety evoked by DOI, did not contribute to hallucinations, highlighting that psychedelics target different parts of the brain to drive many behavioral changes.
Neuronal Mechanisms Behind DOI’s Effects
Electrophysiological studies revealed that the psychedelic DOI increased the firing of parvalbumin-positive, fast-spiking, interneurons in the ventral hippocampus, which express the serotonin2A receptor. This identified the potential cellular trigger through which the psychedelic DOI may reduce anxiety behavior.
To behaviorally test this, chemogenetic strategies were used to activate this particular subclass of neurons within the ventral hippocampus in the absence of the psychedelic DOI, which was sufficient to decrease anxiety behavior in animal models. Further, using a genetic knockout mouse model that lacked any serotonin2A receptor in the brain and body, selective restoration of the serotonin2A receptor on parvalbumin neurons was sufficient to reinstate the decline in anxiety that was seen on treatment with the psychedelic DOI in the ventral hippocampus.
Together, using genetic, pharmacological, electrophysiological, and behavioral studies, the team identified parvalbumin-positive, fast-spiking, interneurons in the ventral hippocampus as the cellular trigger through which the psychedelic DOI can reduce anxiety.
This provides the first evidence of a clear mapping of the precise neuronal population and brain region targeted by a psychedelic to influence anxiety behavior. Since it also demonstrated that this brain circuit does not evoke altered perception and hallucinations, it opens up the intriguing possibility of using psychedelic-inspired drugs that have therapeutic potential for the treatment of anxiety disorders, whilst not exerting potent hallucinatory effects.
Reference: “Ventral hippocampal parvalbumin interneurons gate the acute anxiolytic action of the serotonergic psychedelic DOI” by Praachi Tiwari, Pasha A. Davoudian, Darshana Kapri, Ratna Mahathi Vuruputuri, Lindsay A. Karaba, Mukund Sharma, Giulia Zanni, Angarika Balakrishnan, Pratik R. Chaudhari, Amartya Pradhan, Shital Suryavanshi, Kevin G. Bath, Mark S. Ansorge, Antonio Fernandez-Ruiz, Alex C. Kwan and Vidita A. Vaidya, 24 September 2024, Neuron.
DOI: 10.1016/j.neuron.2024.08.016
Funding: Department of Atomic Energy, Sree Padmavathi Venkateswara Foundation (SreePVF), Vijayawada, Andhra Pradesh (V.A.V.), NIH/NIMH Grants, One Mind—COMPASS Rising Star Award (A.C.K.), NIH/NIDA Fellowship, NIH/NIGMS Medical Scientist Training Grant, NIH Grant, Sloan Fellowship, Whitehall Research Grant, Klingenstein-Simons Fellowship (A.F.-R), NIH Grants, NIH Grant, Sackler Institute Award and NIH Grant, National Science Foundation Graduate Research Fellowship Grant