New research reveals the upper intestinal epithelium’s key role in celiac disease’s immune response, suggesting potential new treatment approaches that target this early-stage interaction.
Celiac disease is a hereditary autoimmune disorder that affects approximately 1 percent of the population. When people with celiac disease ingest gluten—a protein found in wheat, rye, and barley— it can trigger painful symptoms in the gut, impede the absorption of nutrients, and increase the risk of other serious long-term issues.
Its rate of occurrence has roughly doubled in the past 25 years, but there is no treatment available.
Breakthrough Research in Celiac Disease
For the last six years, a team of medical and engineering researchers centered at Canada’s McMaster University, including colleagues from the US, Australia, and Argentina, has been working to unlock a significant piece of the puzzle in the search for a cure: how and where the gluten response begins.
New Discoveries in Intestinal Response to Gluten
Previously, it was believed that the inflammatory response to gluten occurred inside the gut wall and exclusively involved immune cells. However, in a new paper published in the journal Gastroenterology, the team has revealed there is more to the story.
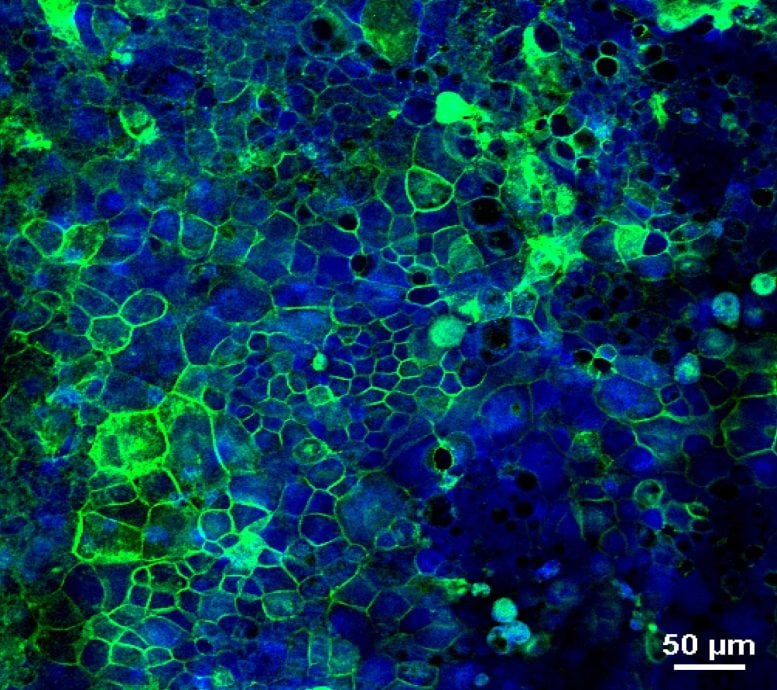
They found that the inner lining of the upper intestine called the “epithelium” –composed of a variety of cells that are not classically part of the immune system – also plays an active role in directing the inflammatory response to gluten.
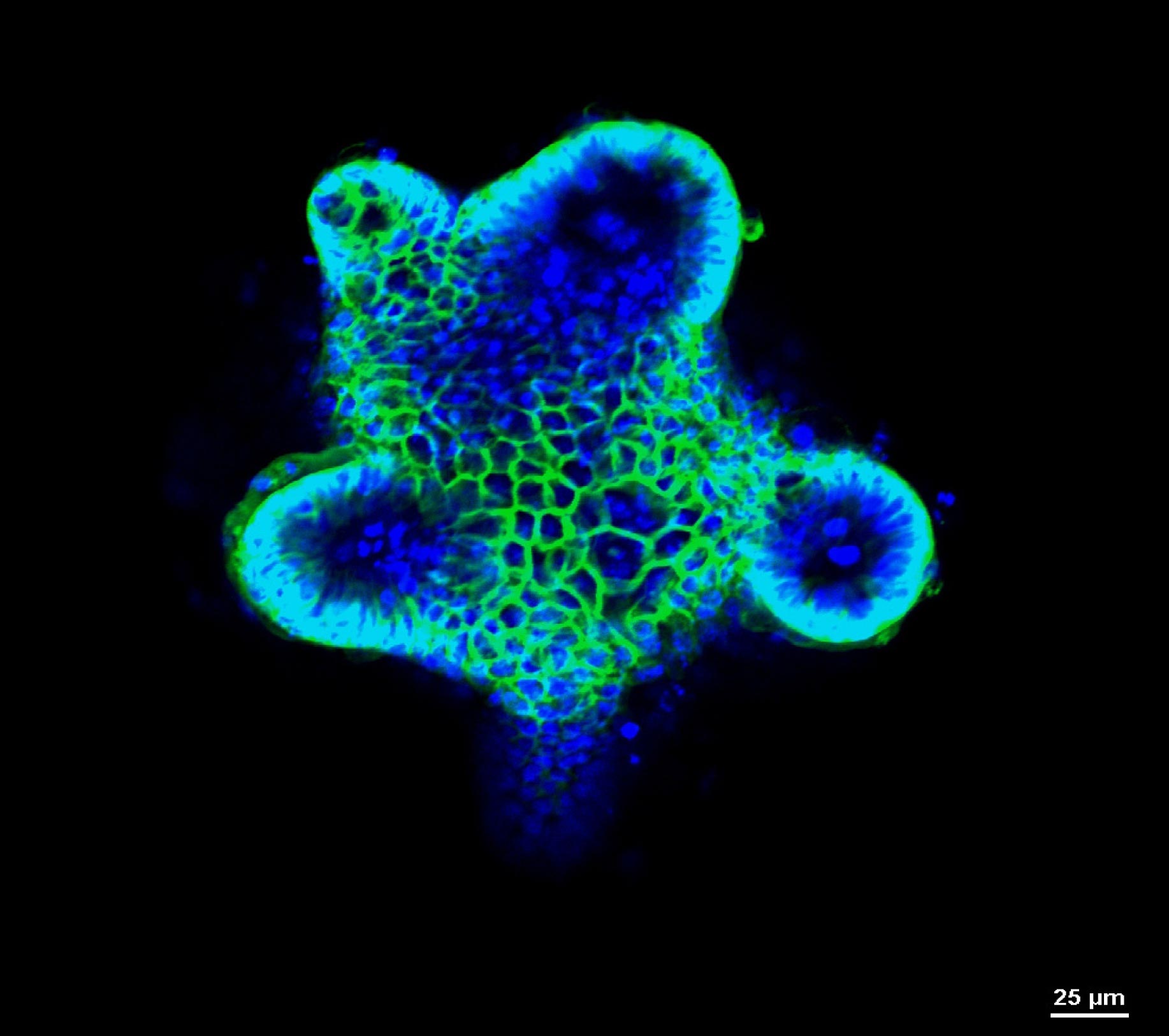
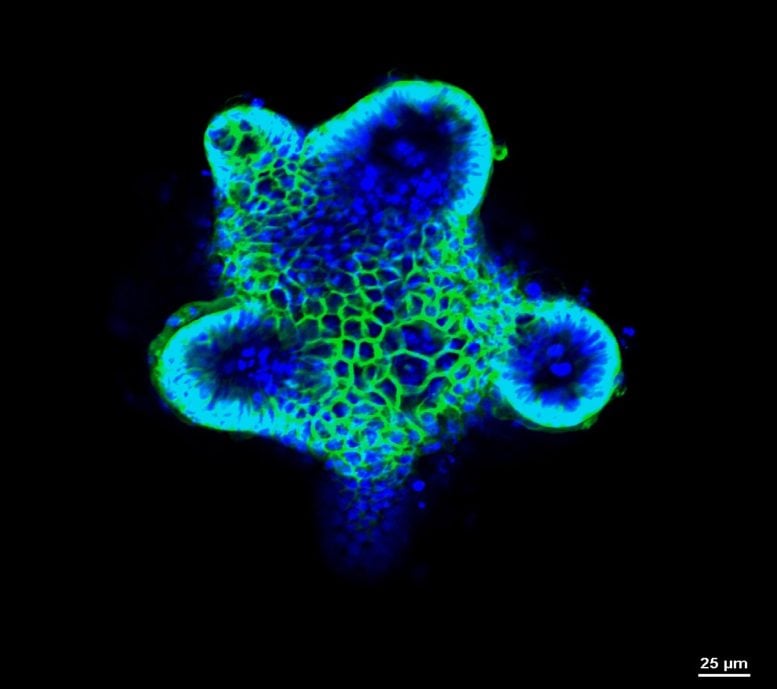
Using microscopic biomaterials in the laboratory, the team created a biologically functioning model of the intestinal epithelium which allowed the researchers to isolate the effects of specific molecules in the epithelial cells of people with celiac disease.
The model allowed the researchers to generate and observe the reactions under controlled conditions, an option that is simply not available in extremely complex gut environments of living beings.
They were able to observe how the molecules alert immune cells to the presence of gluten and to conclude definitely that the epithelium plays a crucial role in activating the immune system in celiac disease.
Such a mechanism had been postulated before but was never proven. Answering this controversial question is expected to advance the development of new drugs.
Advancements in Celiac Disease Research and Future Treatments
“The only way we can treat celiac disease today is by fully eliminating gluten from the diet. This is difficult to do, and experts agree that a gluten-free diet is insufficient,” says Elena Verdu, a corresponding author on the paper who is a professor of gastroenterology and director of McMaster’s Farncombe Family Digestive Health Research Institute.
Precisely locating the spark of the immune response could stimulate research into drug delivery to inhibit this newly found role of the epithelium, using drugs already in clinical trials, Verdu says.
“This allowed us to narrow down the specific cause and effect and prove exactly whether and how the reaction takes place,” says Tohid Didar, a corresponding author on the paper and an associate professor at McMaster’s School of Biomedical Engineering who holds the Canada Research Chair in Nano-biomaterials.
Another significant finding from the study is that after detecting gluten, the epithelium sends stronger signals to immune cells if pathogens are also present.
This means that In the future it may be possible to detect the pathogen in a person at risk of developing the disease, and inhibit the interactions with gluten and the gut epithelium to prevent the disease, says the paper’s lead author, Sara Rahmani, a PhD candidate in the Verdu and Didar labs.
Reference: “Gluten-Dependent Activation of CD4+ T Cells by MHC Class II–Expressing Epithelium” by Sara Rahmani, Heather J. Galipeau, Alexandra V. Clarizio, Xuanyu Wang, Amber Hann, Gaston H. Rueda, Utkarshini N. Kirtikar, Marco Constante, Mark Wulczynski, Hsuan-Ming Su, Rebecca Burchett, Jonathan L. Bramson, Maria Ines Pinto-Sanchez, Juan Pablo Stefanolo, Sonia Niveloni, Michael G. Surette, Joseph A. Murray, Robert P. Anderson, Premysl Bercik, Alberto Caminero, Fernando G. Chirdo, Tohid F. Didar and Elena F. Verdu, 9 August 2024, Gastroenterology.
DOI: 10.1053/j.gastro.2024.07.008