By the Numbers: A rising fatality rate.
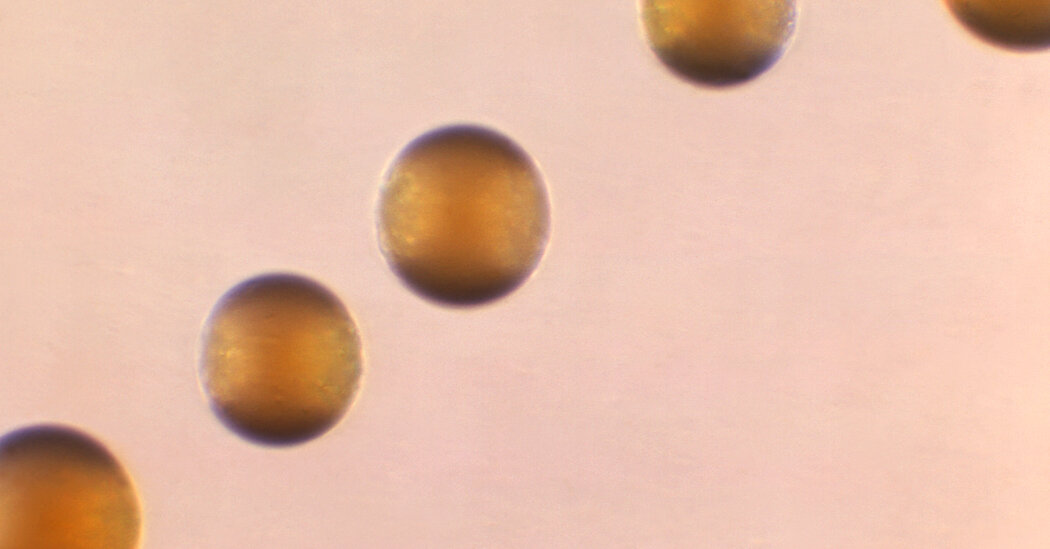
The illness is caused by infection with a bacterium called Neisseria meningitidis. Last year, 422 cases of invasive meningococcal disease were reported in the United States, the highest number since 2014, according to the Centers for Disease Control and Prevention.
But as of Monday, 143 cases have been reported to the C.D.C. so far this year, 62 more than the number of cases reported last year during the same period.
The illness is extremely dangerous. Even with appropriate treatment, 10 to 15 percent of patients who develop meningococcal disease will die. Many recent cases were caused by an unusual strain of N. meningitidis called ST-1466. This strain caused 17 deaths among 94 patients whose outcomes are known, a fatality rate of 18 percent.
Survivors of meningococcal disease may be left with long-term disability, deafness, amputations or brain damage.
The Mystery: What’s causing the outbreaks?
A majority of people affected in the recent outbreaks were Black people and adults ages 30 to 60.
Others who are susceptible to the infection include people living with H.I.V., who account for 15 percent of patients; individuals who have had their spleens removed; people with sickle cell disease; and patients with certain rare immune conditions.
A meningitis vaccine that protects against four of six N. meningitidis types — including group Y, which includes ST-1466 — is recommended for adolescents as well as those with medical conditions like H.I.V. Most older adults have not received the vaccine.
In Virginia, which has had 35 cases of meningococcal disease and six deaths since the summer of 2022, public health officials have not found an epidemiologic link that explains the outbreak, said Dr. Laurie Forlano, the state’s epidemiologist.
“We always try to find that golden ticket of common risk factors,” Dr. Forlano said. “Were they all at one party together, or at one family event? Were they all at a certain facility? Are there social networks they share? That’s just not the case here.”
The illness is not spread through casual contact, but through activities that involve exposure to saliva or respiratory or throat secretions — kissing, for example, or sharing food and drinks or cigarettes.
A Ticking Clock: Treatment must happen quickly.
The infection can cause meningitis, an inflammation of the membranes covering the brain and spinal cord. Typical symptoms include fever, headaches, stiff neck, vomiting, light sensitivity and altered mental status.
The bacteria can also invade the bloodstream, a complication called sepsis, which appears to be the more common consequence with the current serogroup Y cases. Symptoms include fever and chills, fatigue, vomiting, cold hands and feet, severe aches and pains, diarrhea, rapid breathing and, in later stages, a dark purple rash.
Symptoms may intensify rapidly and become life-threatening in a matter of hours. Antibiotics must be administered promptly.
“With meningococcal disease, people’s thoughts go to meningitis, which is a very scary condition,” Dr. Forlano said. “But the point we’re trying to make to the clinical community is that these cases are presenting differently to what we’re used to seeing. So, hey, think about this.”
Despite the risk, however, she emphasized that the illness remains rare. “The threat to the general public is low,” she said.