Every region of Ontario is experiencing a shortage of family doctors and the crisis is only going to get worse if the provincial government doesn’t take immediate action, the Ontario Medical Association (OMA) is warning.
The number of Ontario residents who don’t have a family doctor — currently sitting around 2.3 million people — is expected to nearly double in the next two years, the OMA said in a news release Monday. The OMA represents over 43,000 physicians, medical students and retired physicians in the province.
“The implications of people not being able to access primary care are severe,” OMA president Dr. Andrew Park said in the release.
Park warned the situation in Sault Ste. Marie — where a long-standing health-care centre said last week it would drop 10,000 patients from its roster by May because of a doctor shortage — could replicate itself across the province.
“We can’t just sit back and watch this situation get worse. We need to act now so people in Ontario can get care when they need it,” Park said.
The warning underscores the severity of the province’s doctor shortage, which worsened during the COVID-19 pandemic when hundreds of family doctors stopped practising. It’s poised to grow further still with many aging baby-boomer doctors planning to retire.
More than 2,500 open doctor jobs
More than 2,500 physicians are needed across the province, the association said, citing open job postings on HealthForceOntario, which post job openings for doctors. Toronto has the largest number of openings at 305, followed by Ottawa with 171, the Barrie and Muskoka Region with 118 and Hamilton at 114, according to the data.
An OMA survey of its members suggests that 40 per cent of physicians are considering retiring in the next five years. The association said “underfunding” in OHIP revenue and rising costs due to inflation are making family practices unsustainable. In addition, family doctors report spending 40 per cent of their work week on completing forms and trying to navigate patients through a system that is disconnected and fragmented, the association said.
Dr. Jobin Varughese, president-elect of the Ontario College of Family Physicians, said the number of medical students choosing family medicine as a specialty is declining because the financial compensation isn’t as fruitful compared to other specialties.
“Office-based practice, being in a clinic and being able to spend time with your patients, that should be a valued and well-compensated model and right now it’s not,” Varughese said. “We need to make family medicine a valued specialty.”
The OMA said it wants to see the province expand access to team-based care and reduce the burden of unnecessary administration facing doctors.
Varughese said reducing the amount of paperwork doctors must complete will increase the time they can spend with their patients. On the other hand, connecting family doctors to medical teams that could include nurse practitioners and administrative assistants will help them feel more supported in their work.
“When you get to a situation that you have a whole lot of tasks that don’t let you see patients and you have a whole bunch of situations that you’re left on your own, it gets very difficult to really handle that and we’re seeing a lot of burnout,” he said.
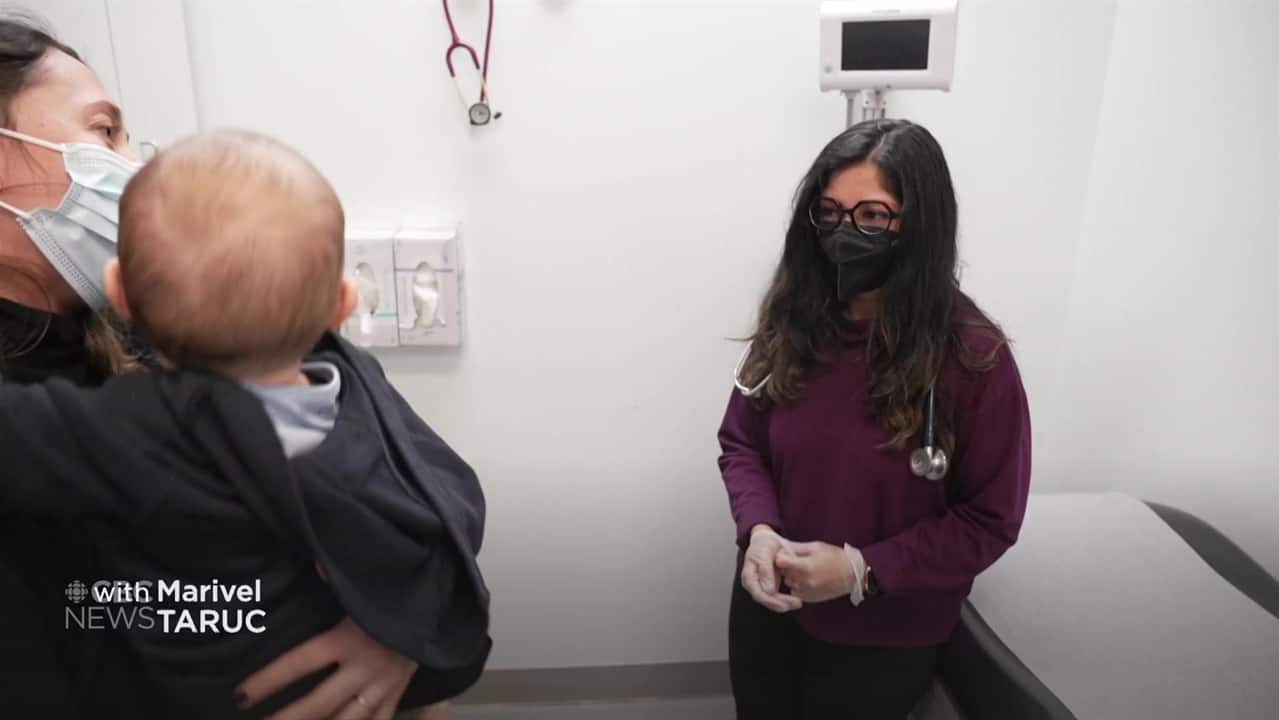
Inside the Village Family Health Team in Toronto, where family physicians work alongside nurses and other health professionals.
Move comes amid contract talks with province
The OMA’s warning also comes as the OMA and the Ministry of Health are engaged in negotiations over the next physician services agreement, which determines how much money physicians can bill the government for providing care under OHIP. The current agreement expires on March 31, 2024.
The Ontario Union of Family Physicians (OUFP), a group of approximately 1,700 family doctors that is advocating for reform to make family medicine more sustainable, said some of its members will be taking a “co-ordinated day off” on Feb. 5.
The group says it’s in response to the province’s “inaction” on the primary care crisis and the “lack of goodwill” in negotiations over the physician services agreement.
Dr. Ramsey Hijazi, a family physician in Ottawa who is a lead organizer with the group, says it’s not a strike, but a co-ordinated day off to have a meeting with its members to discuss alternative career paths, which could include moving to different provinces or countries, pivoting to hospital medicine, or making the switch to private aesthetic medicine, among other options.
“Ontario is no longer a safe place to practise family medicine or to set up a new family medicine practice,” said Hijazi.
“It’s just no longer a feasible or viable business.”
Many Canadians still don’t have access to a family doctor. CBC’s Omar Dabaghi-Pacheco explores short-term and long-term solutions to the problem.
Province expanding medical school seats, reducing administrative burden
Hannah Jensen, a spokesperson for Health Minister Sylvia Jones, said in a statement that the provincial government has added more than 10,400 new doctors since 2018.
The government has also expanded medical school access by adding hundreds of undergraduate and medical seats, Jensen said, with 60 per cent of seats reserved for family medicine.
“While Ontario is leading the country with 90 per cent of Ontarians having a primary care provider, we understand that a key part of our Your Health plan is to ensure all Ontarians who want access to primary care are able to,” Jensen wrote.
“That is why we are investing tens of millions of dollars to launch the largest expansion of new interdisciplinary primary care teams.”
Jensen said the government is working to reduce the administrative burden on doctors through the Bilateral Burnout Task Force, a joint committee involving both the Ministry of Health and the OMA that was created in 2022 to address burnout among physicians.
The task force has already “significantly accelerated work” to simplify forms doctors must fill out, Jensen said, and the government is also seeking to replace fax machines at all Ontario healthcare providers with digital alternatives, to streamline communications.
When asked about the OUFP’s co-ordinated day off, Jensen said, “We look forward to continued discussions at the table with the OMA.”