The long-awaited NHS workforce plan to address a staff shortfall of up to 360,000 healthcare workers was today unveiled by the health service.
Backed by a £2.4bn investment from the Government over 15 years, the package of measures aims to tackle chronic staff shortages and the rise in demand from England’s growing and ageing population.
The Government claims the plan will also help slash record waiting lists for patients.
But critics warn the blueprint has failed to address staff retention, with much of the workforce tired and burnt out following gruelling Covid pressures.
So what does the full plan propose? How many more healthcare workers will join the NHS? What will happen to medical degrees? And how will it be funded?
Here MailOnline explains everything you need to know about the first-ever NHS long-term workforce plan.
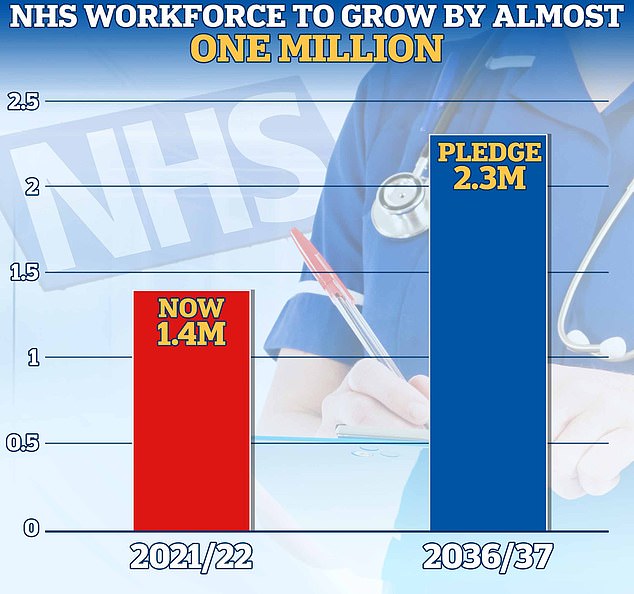
The plan has pledged to increase the NHS permanent workforce by almost a million by 2036/2037. It expects to see a rise from 1.4million to between 2.2 and 2.3million




The number of medical school training places will be doubled by 2031/32, taking the total number of places to 15,000. GP training places in England for junior doctors will also increase by 50 per cent to 6,000, the NHS’s workforce plan has pledged. Training for pharmacists will also rise by almost 50 per cent to around 5,000 places for 2031/32. Meanwhile, training for clinical psychology and child and adolescent psychotherapy will also be expanded, with places rising by more than a quarter to 1,300 by 2031
How many more medics will join the NHS?
The plan has pledged to increase the NHS permanent workforce by almost a million by 2036/2037.
It expects to see a rise from 1.4million to between 2.2 and 2.3million.
This will include between 60,000 and 74,000 more doctors, up from the 142,000 working for the health service as of this month.
How has it pledged to increase the number of nurses and midwives?
The plan will also see the number of nurses increase between 170,000 and 190,000, rising from the 370,000 reported this month.
There will also be a five-fold rise in assistant roles, such as nurse and physician associates.
But Sara Gorton, head of health at the union, Unison, also warned: ‘Plans to recruit more Drs. and nurses can’t ignore the NHS shortage of porters, cleaners, 999 call handlers & other support roles.
‘Non-clinical staff are most at risk of leaving the NHS for better paid, less stressful jobs.’
How does the plan affect primary care?
Under the workforce plan, the number of non-GP direct patient care staff will rise by around 15,000 and primary care nurses by more than 5,000 by 2036/37.
Experienced doctors will also be supported to work in general practice under the supervision of a fully qualified GP, the health service said.
‘We will also ensure that all foundation doctors can have at least one four-month placement in general practice, with full coverage by 2030/31,’ they added.
The health service will also support 3,000 existing pharmacists to become independent prescribers, allowing them to prescribe medications directly.
How many more allied health professionals will join the health service?
The plan has pledged to increase the allied health professional workforce by between 71,000 and 76,000 by 2036/37.
Some 14 different roles sit under allied health professions.
These include podiatrists, physiotherapists, paramedics, radiographers, speech and language therapists and dieticians.
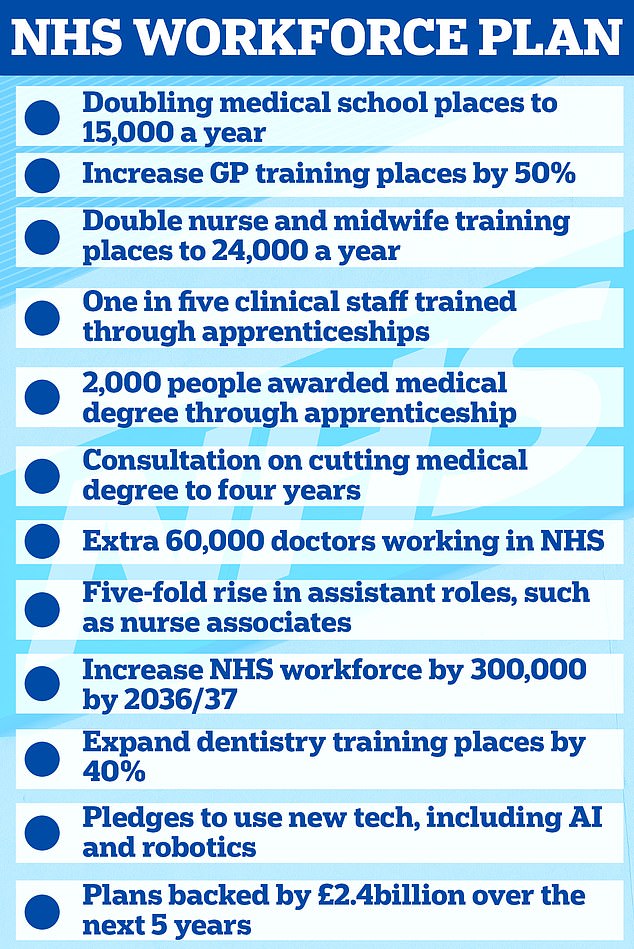
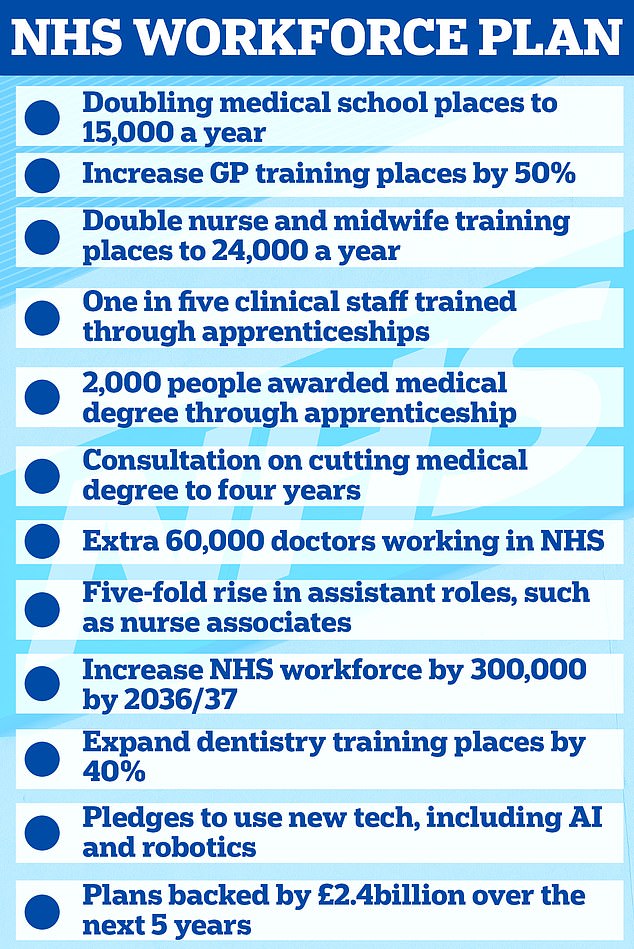
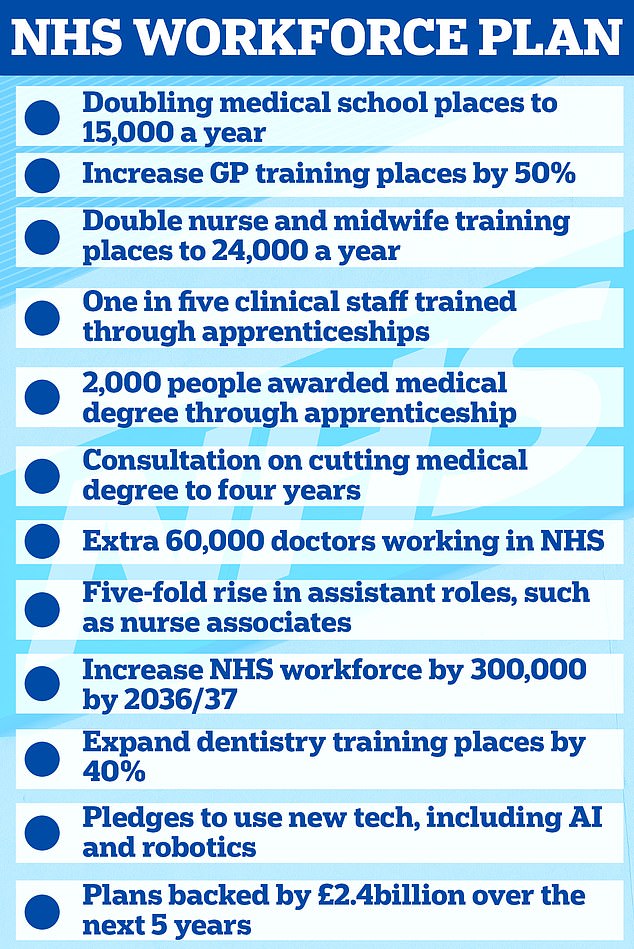
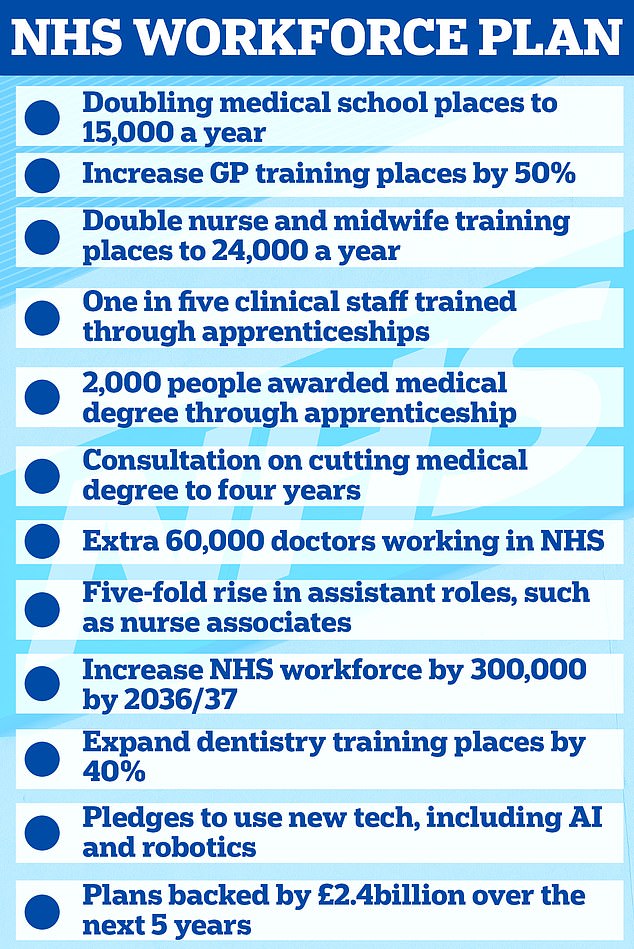
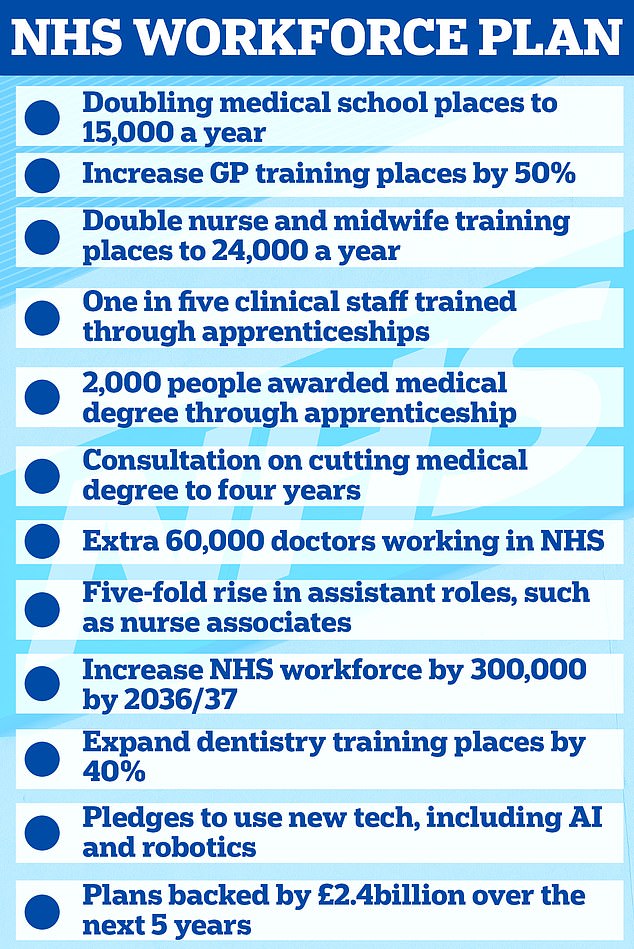
The ambitious proposals are detailed in the first NHS Long-Term Workforce Plan, which is published today and supported by £2.4billion of Government funding
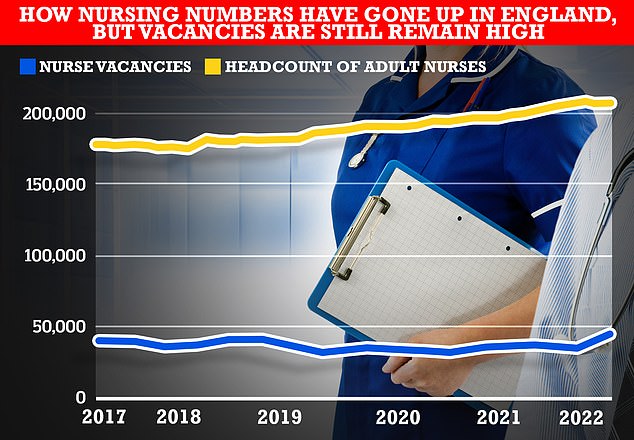
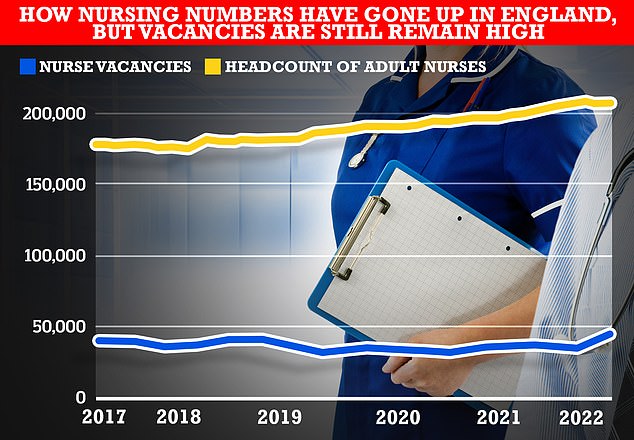
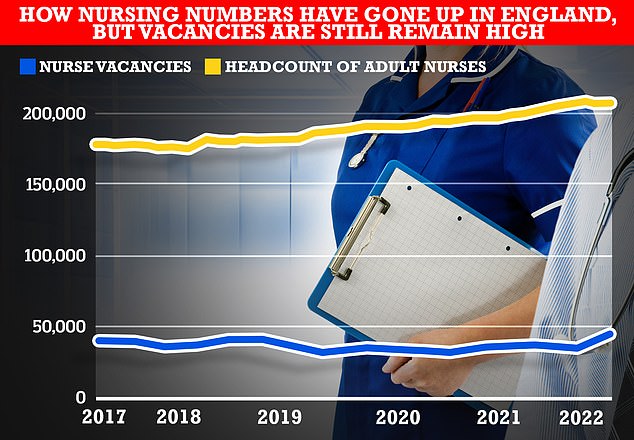
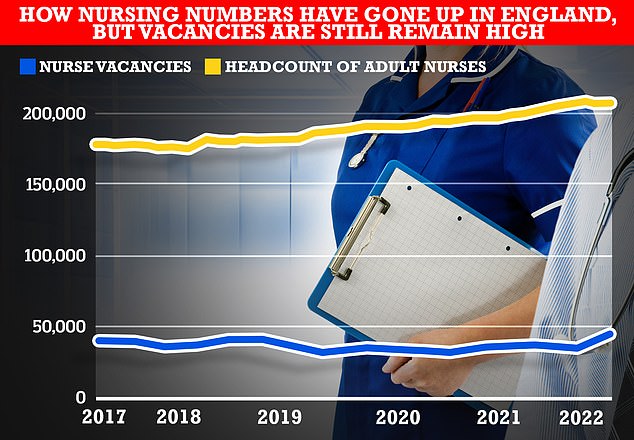
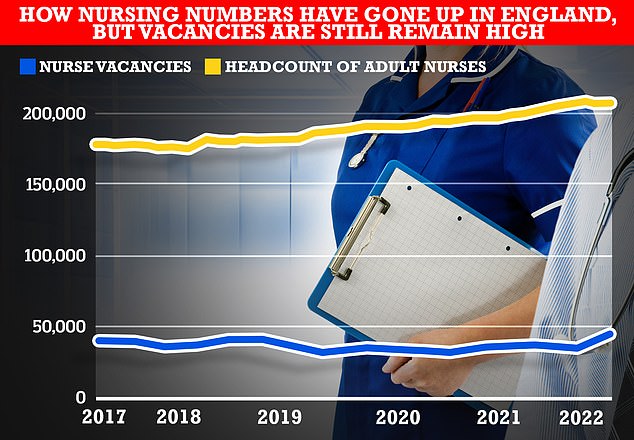
While the headcount of full-time-equivalent adult nurses, who account for most nurses in the NHS in England, has gone up the number of total nursing vacancies has remained stubbornly high, official figures show. This has left the NHS essential treading water in terms of addressing staffing shortages
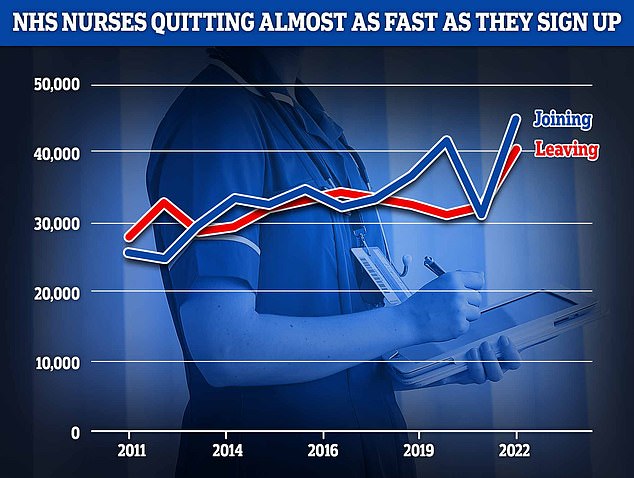
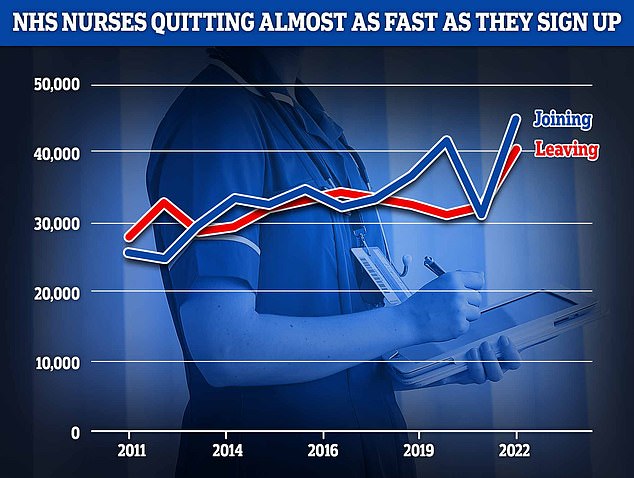
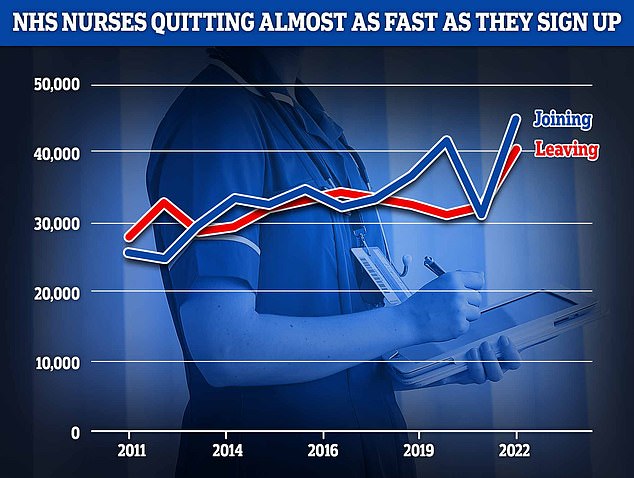
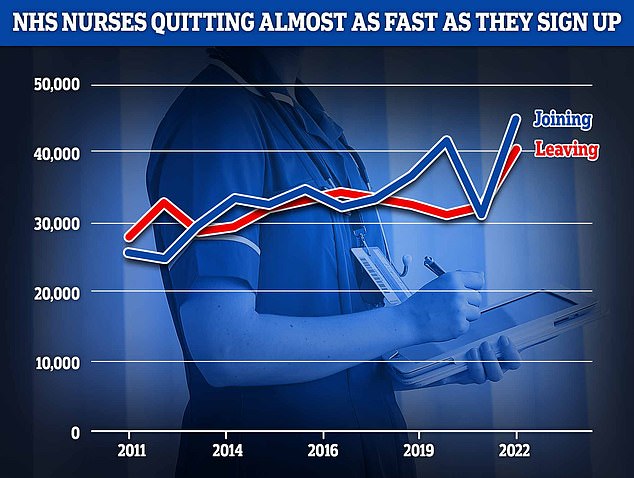
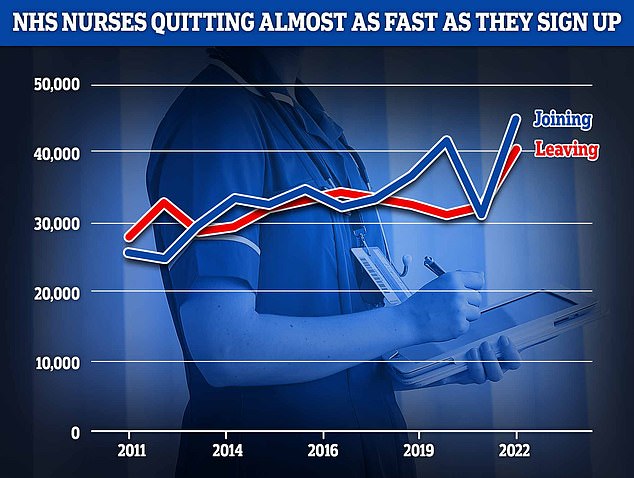
NHS data shows efforts to get more nurses into the health service are only barely keeping pace with the number of experienced nurses quitting
How does the plan propose increasing the number of dentists?
NHS dentistry has been in crisis for many years, with industry leaders saying the sector has been chronically underfunded.
Thousands of NHS dentists quit during Covid, and industry polls suggest even more are considering going fully private in the near future.
Dentists argue that under the current contract, it is no longer financially viable to offer NHS procedures because of a lack of Government investment.
Under the workforce plan NHS England said it is ‘reforming contractual arrangements to encourage more dentists back into NHS practice’
This will also make it ‘easier for therapists and hygienists to provide NHS care directly’, they added.
How will mental health services be supported?
The number of approved clinician roles across mental health services will rise by at least 1,000 between 2022/23 and 2036/37.
This includes clinical psychologists, psychological therapists, mental health and wellbeing practitioners, children’s wellbeing practitioners and educational mental health practitioners.
How will the plan be funded?
The 15-year plan will be backed by a £2.4bn investment from the Government.
This will ‘fund additional education and training places over five years on top of existing funding commitments’, NHS England said.
But the commitment will need to be updated every two years as circumstances change, the health service added.
What is happening with training places?
The number of medical school training places will be doubled by 2031/32, taking the total number of places to 15,000.
More medical school places will be offered ‘in areas with the greatest shortages, to level up training and help address geographical inequity’, NHS England said.
To achieve this, medical school places will rise by a third – to 10,000 – by 2028/29, with the first new medical school places available from September 2025.
Adult nursing training places will also rise by 92 per cent, taking the total number of places to almost 38,000 by 2031/32, the plan proposes.
In the next five years, the health service will increase training places to nearly 28,000.
More student nurses will also be able to take up jobs as soon as they graduate in May, the plan proposed.
Instead of waiting until September, this will allow ‘more reaching the frontline and treating patients more quickly’, NHS England said.
GP training places in England for junior doctors will also increase by 50 per cent to 6,000, the NHS’s workforce plan has pledged.
Over the next five years, the number of GP training places will also rise by 25 per cent, with the first 500 new places available from September 2025.
Training for pharmacists will also rise by almost 50 per cent to around 5,000 places for 2031/32.
Meanwhile, training for clinical psychology and child and adolescent psychotherapy will also be expanded, with places rising by more than a quarter to 1,300 by 2031.
Dentistry training places will also expand to 40 per cent, increasing places to over 500 for dental therapists and hygiene professionals, and to over 1,100 for dentists.
The health service will invest in a two-year masters level paramedic programme, allowing future paramedics to enter the workforce in just two instead of three years.
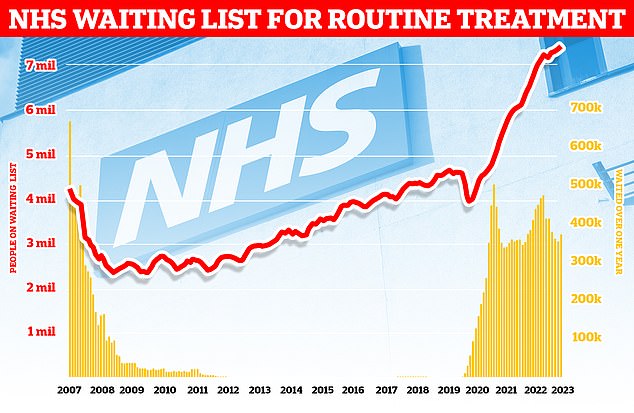
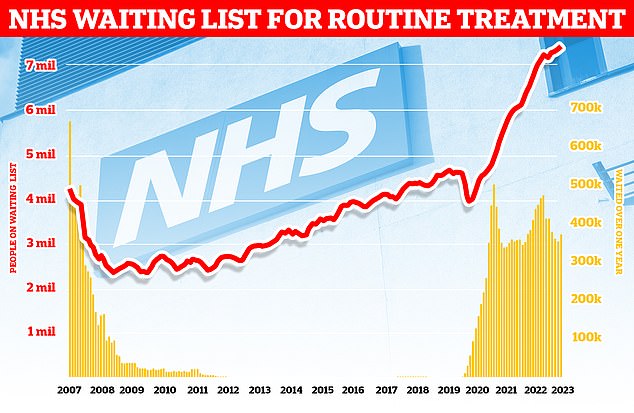
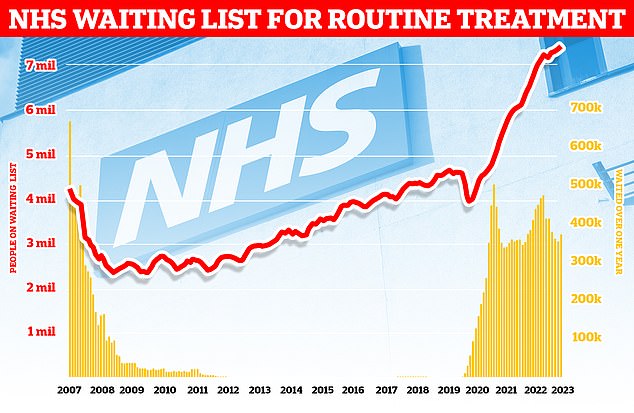
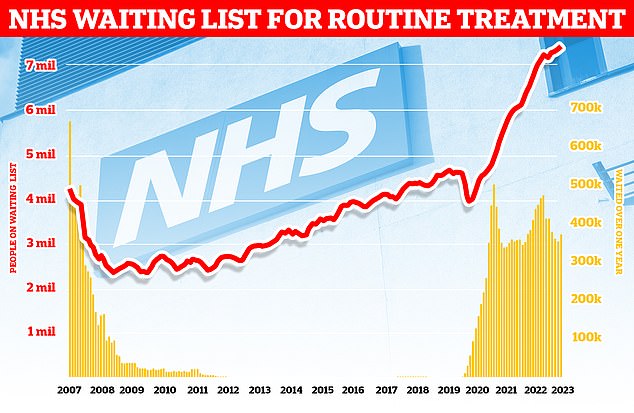
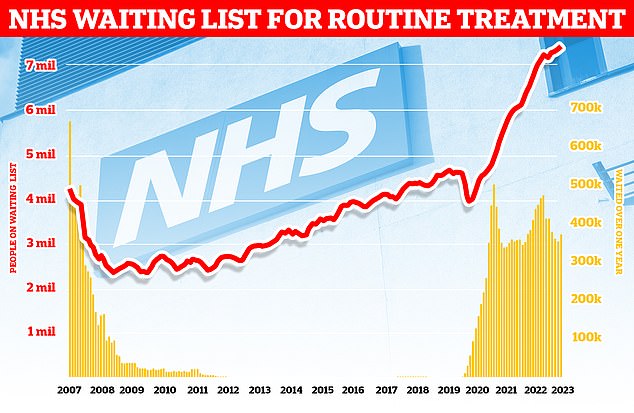
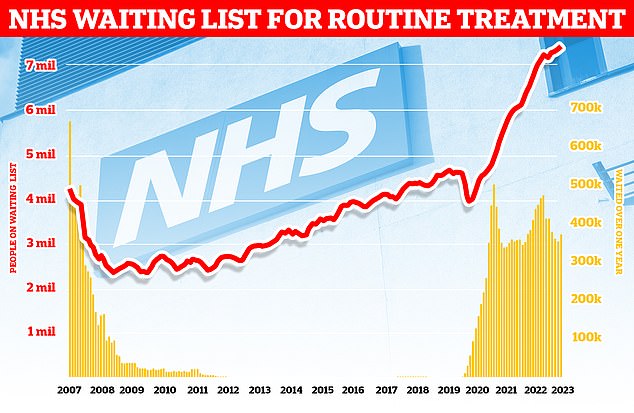
The number of people waiting for routine hospital treatment in England soared to a record 7.42million (red line) in April, figures show. More than 370,000 people in the queue for routine ops, such as hip replacements, were waiting for more than a year (yellow bars)
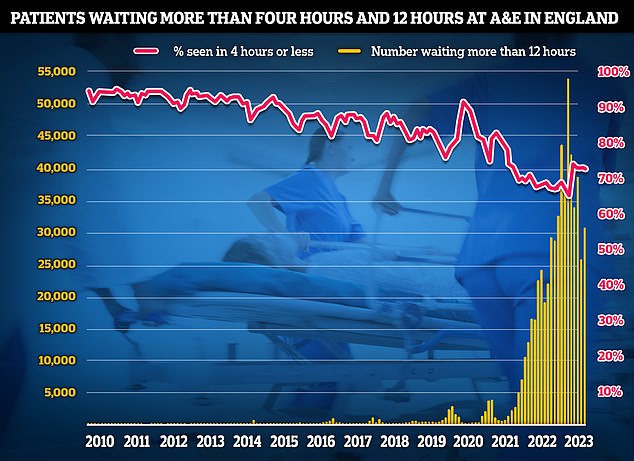
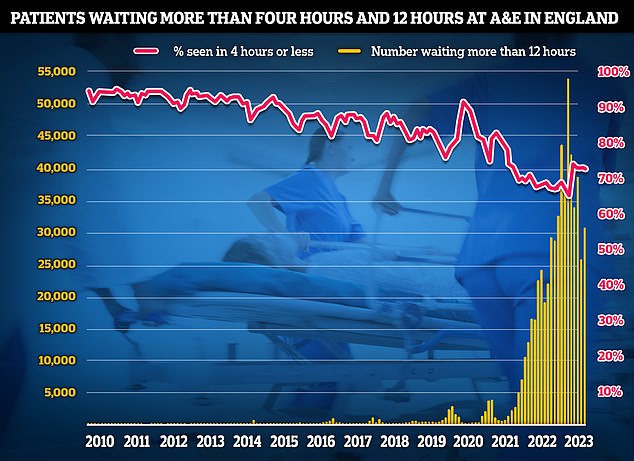
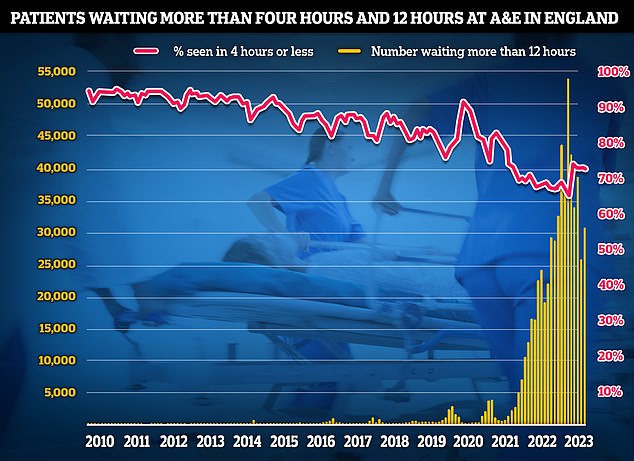
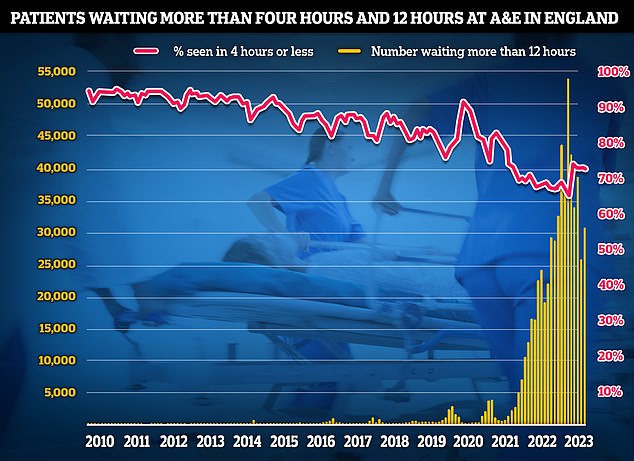
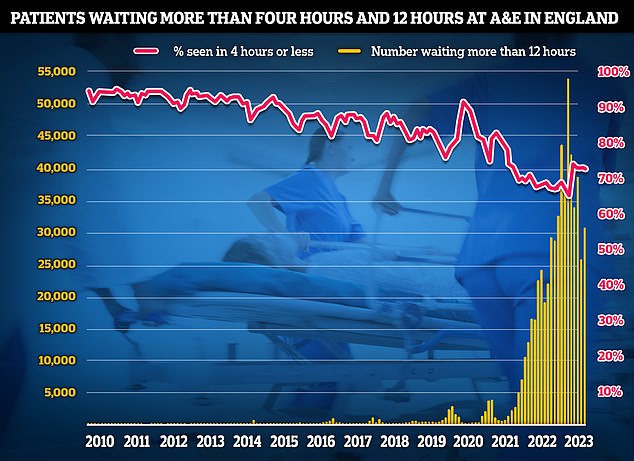
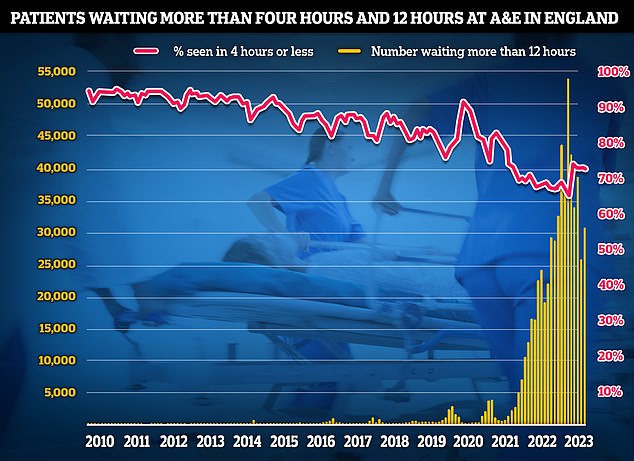
NHS data on A&E performance in May shows that three-quarters of emergency department attendees (74 per cent) were seen within four hours (red line). Meanwhile, 31,494 patients who sought help in emergency departments were forced to wait more than 12 hours — equivalent to more than 1,000 patients per day (yellow bars)
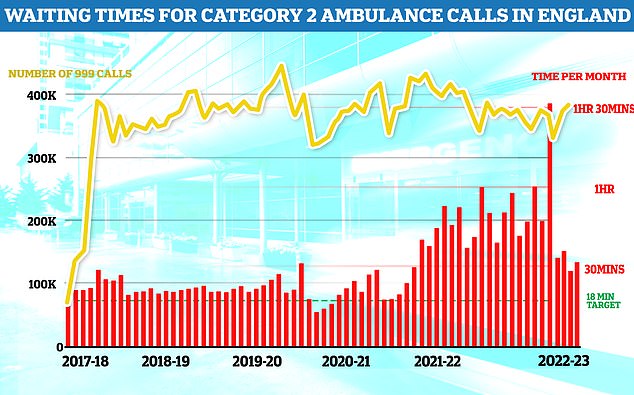
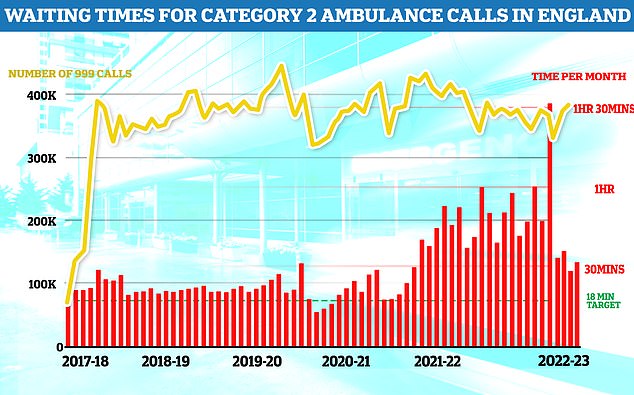
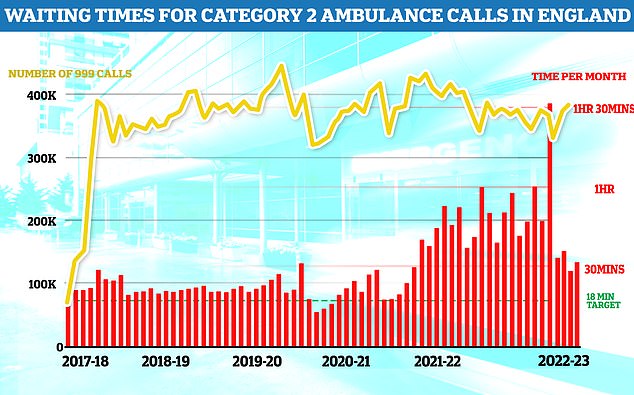
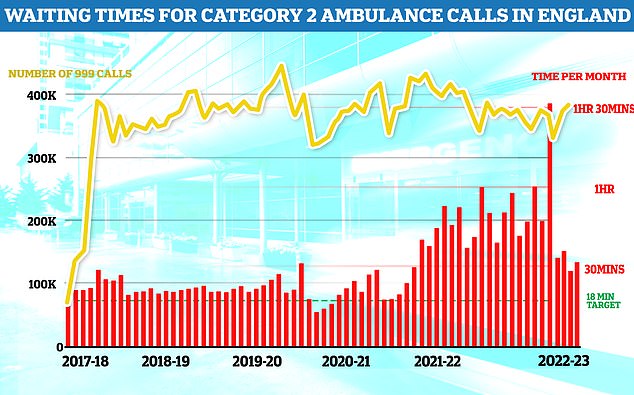
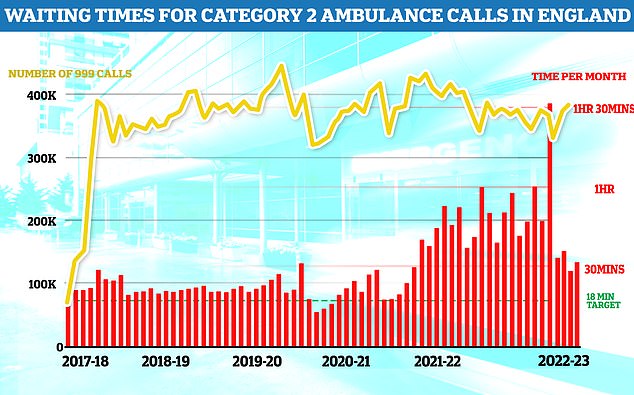
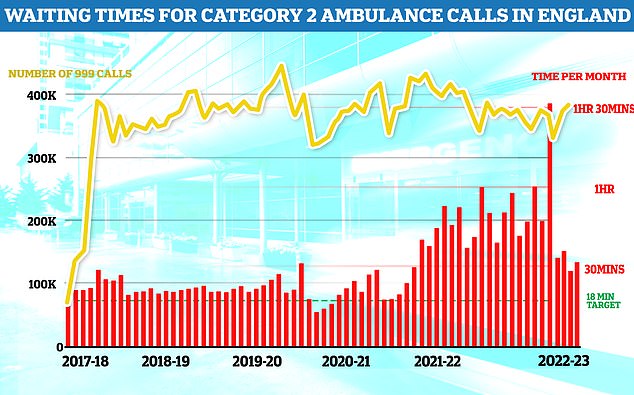
Ambulances took an average of 32 minutes and 24 seconds to respond to category two calls, such as burns, epilepsy and strokes. This is nearly twice as long as the 18 minute target and nearly four minutes longer than one month earlier (red bars)
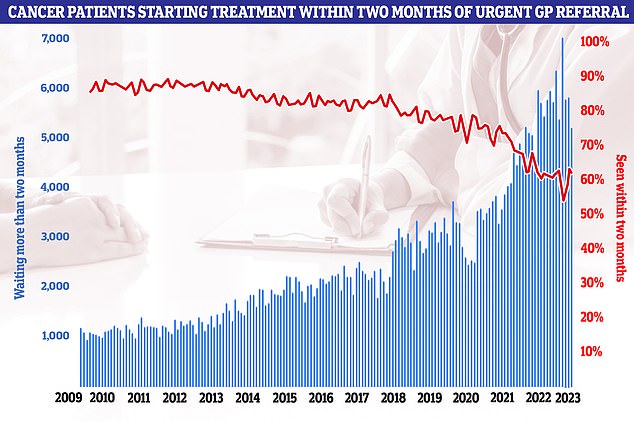
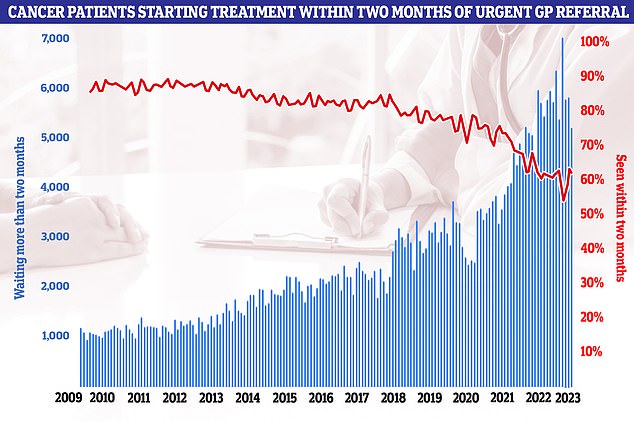
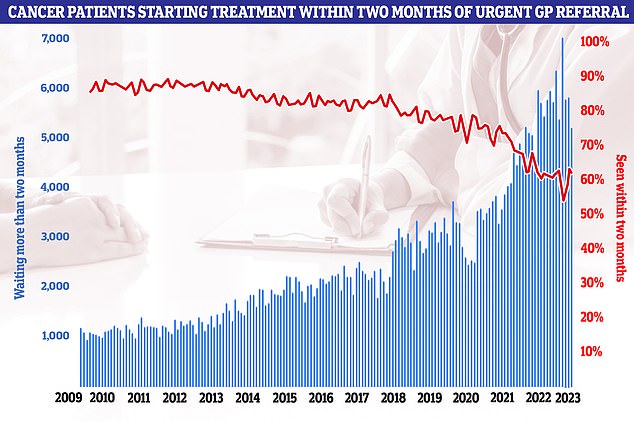
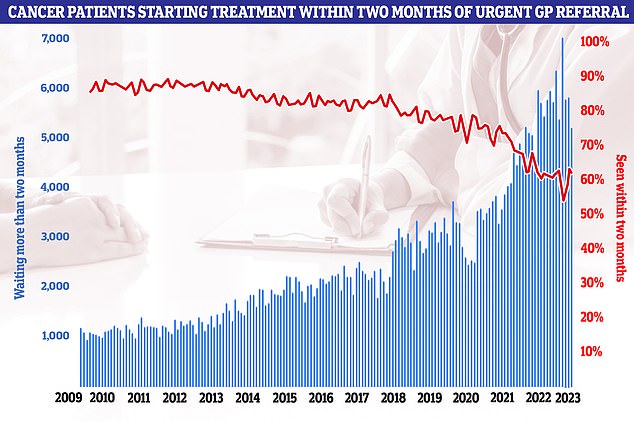
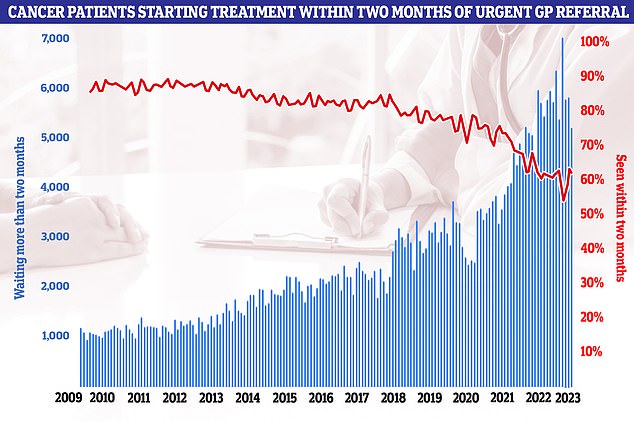
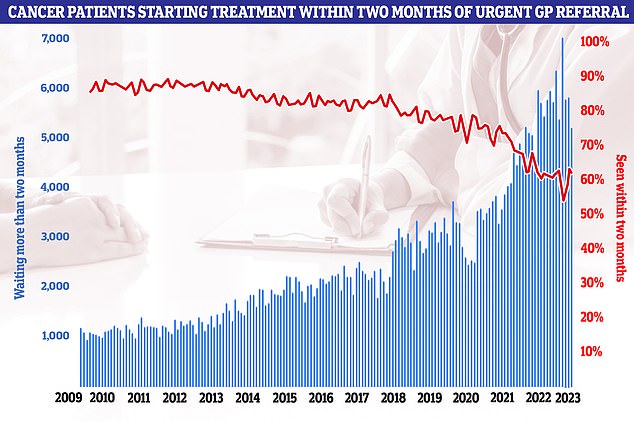
Six in 10 cancer patients started treatment within two months of an urgent GP referral (red line). This is down from March and well below the NHS target of 85 per cent. It means 5,178 patients (blue bars) had to wait longer for surgery, chemo or radiotherapy
What is happening with medical degrees?
The plan also proposes the medical regulator will consider shortening medical degree from five or six-year programmes to four years.
These will ‘meet the same established standards set by the GMC’, the plan proposed, while medical internship programmes will also be piloted.
Trainees ‘will be on wards and in practices sooner’, and will bring medics into the workforce ‘more efficiently’, NHS England said.
New medical schools could open up in areas of the country where there is the greatest staffing shortfall, with similar plans for postgraduate medical training places.
Medical degree apprenticeships will also be introduced, with pilots running in 2024/25.
By 2031/32, NHS England envisions 2,000 medical students will train via this route.
It estimates 850 medical degree apprenticeships will be available by 2028/29.
What is happening with other apprenticeships?
Over a fifth (22 per cent) of clinical staff will be trained through apprenticeships by 2031/32, the document said.
Currently just seven per cent are trained in this way.
In the next five years, this will rise to 16 per cent to ‘ensure we train enough staff in the right roles’, the document said.
‘Apprenticeships will help widen access to opportunities for people from all backgrounds and in underserved areas to join the NHS.’
There is potential to continue expanding training via the apprenticeship route for pharmacy technicians and consideration is being given to the potential of a pharmacist degree apprenticeship.
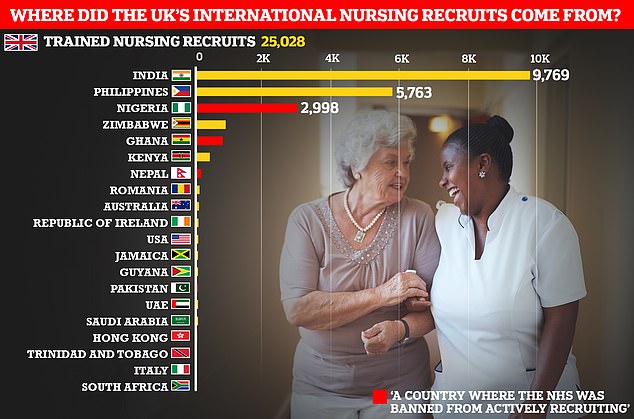
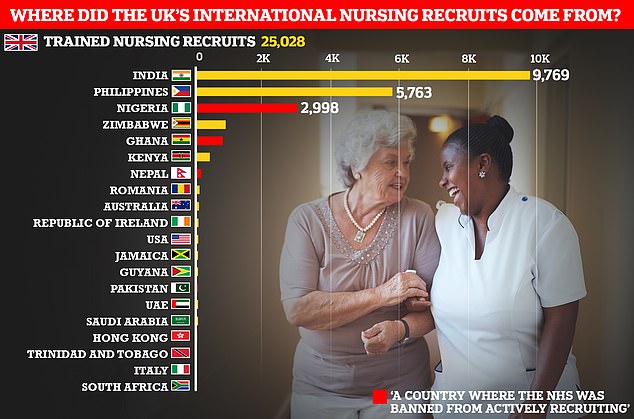
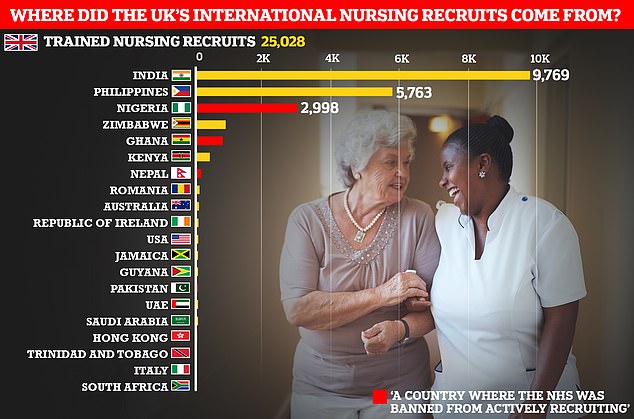
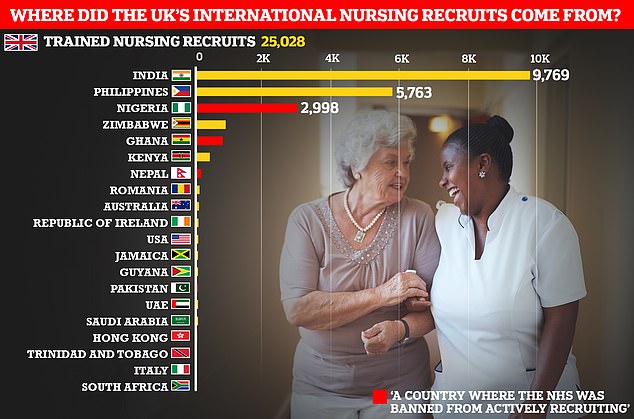
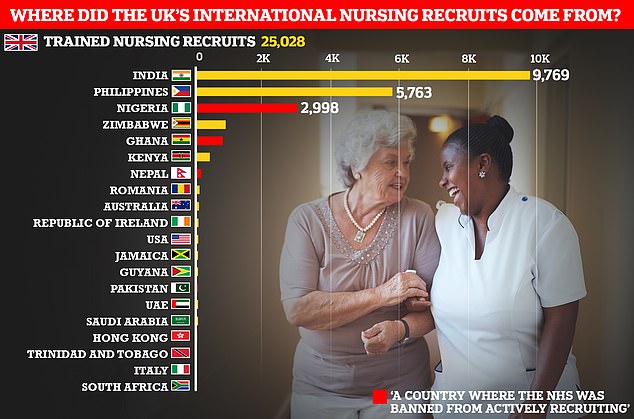
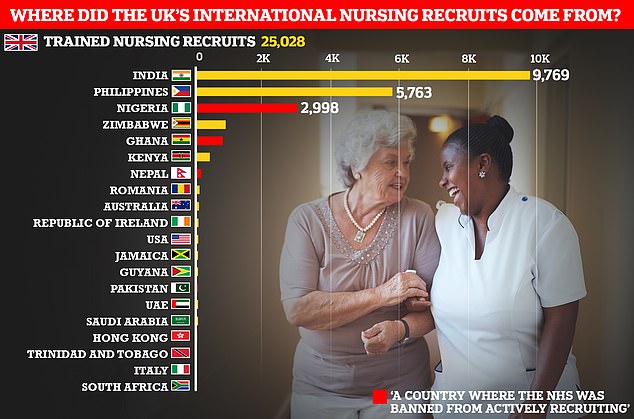
India and the Philippines account for the lion’s share of international nurse recruits for 2021-22 but a fifth came from ‘red listed’ countries where the NHS is banned from actively poaching nurses. These were Nigeria, Ghana, Nepal, and Pakistan. This data, from the UK’s Nursing and Midwifery Council, covers the period before Britain struck a special deal with Nepal to allow the NHS to recruit nurses from the country
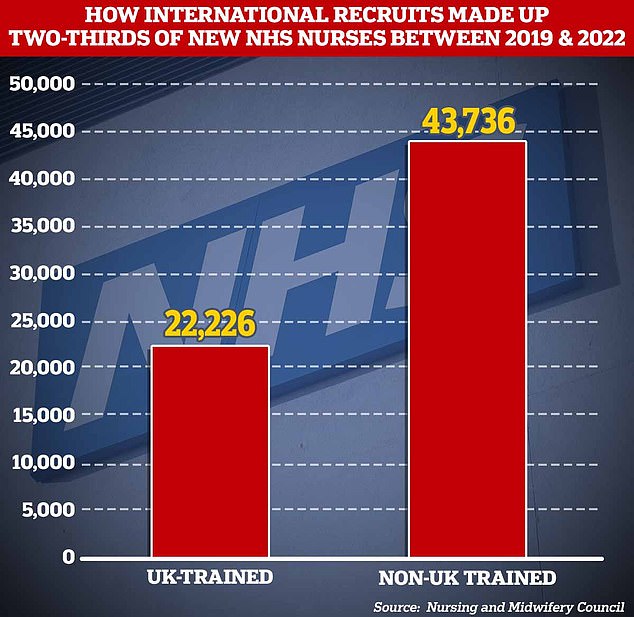
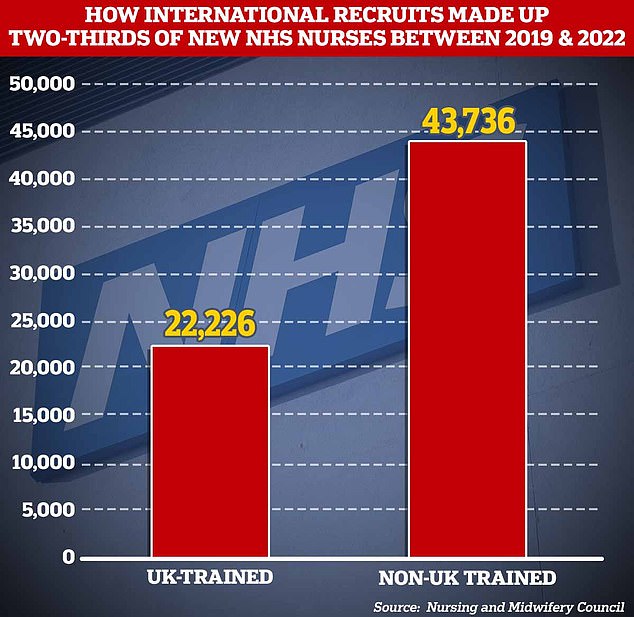
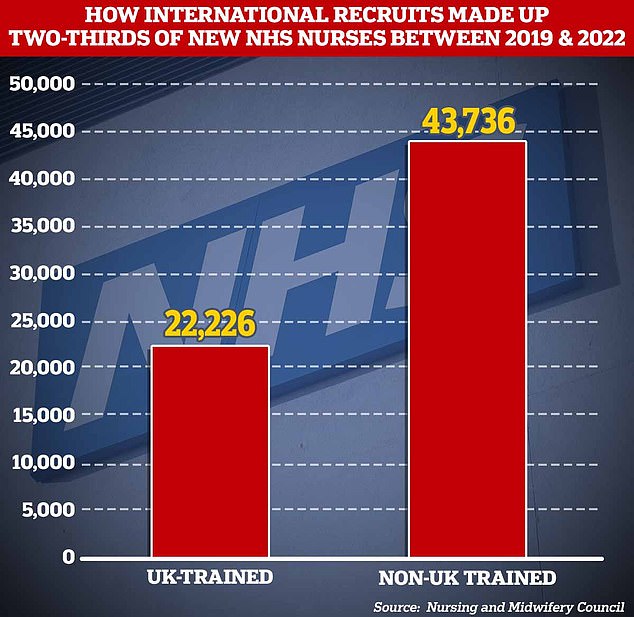
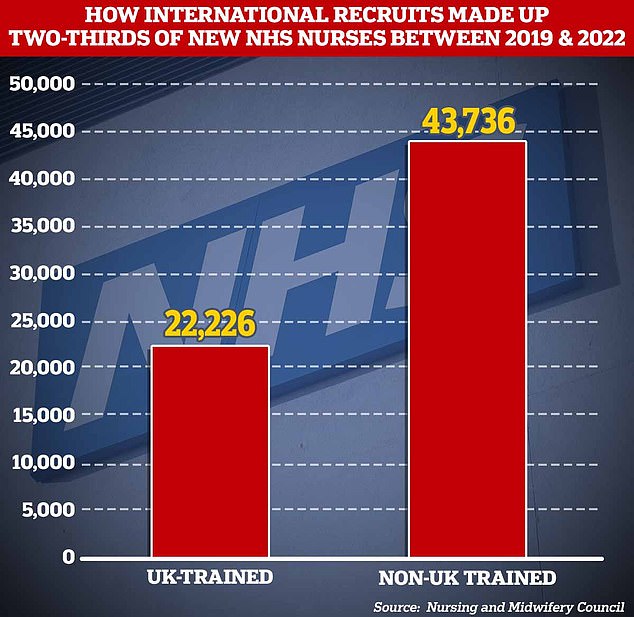
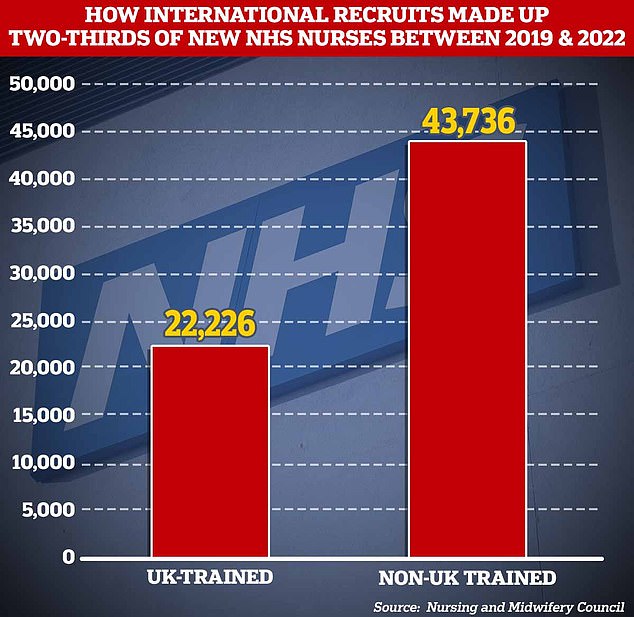
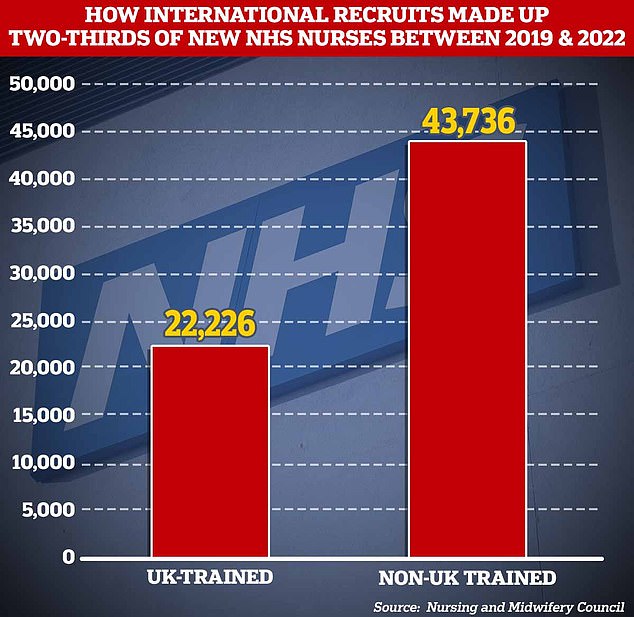
Analysis of the Nursing and Midwifery Council figures by the Nuffield Trust found international recruits account for two-thirds of all new nursing and midwifery staff in the three years since September 2019. Despite falls in the number of staff from the EU, some 43,736 recruits were non-UK staff, while just 22,226 had been trained in the UK
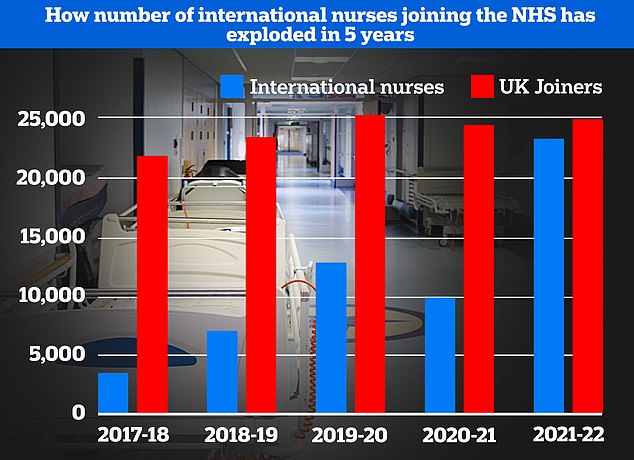
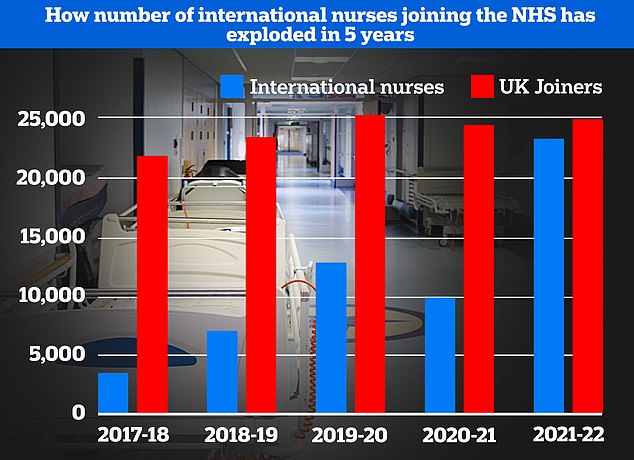
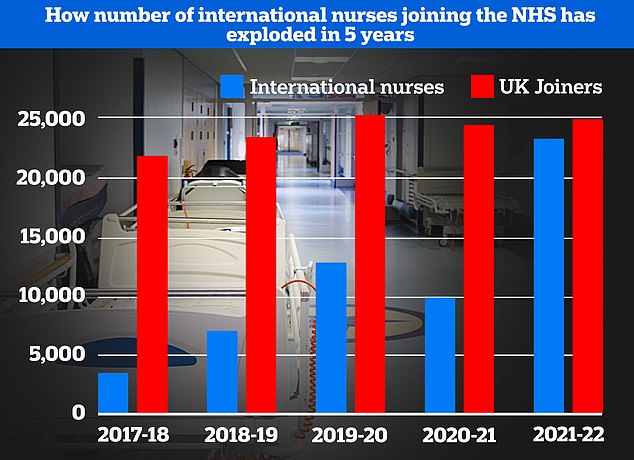
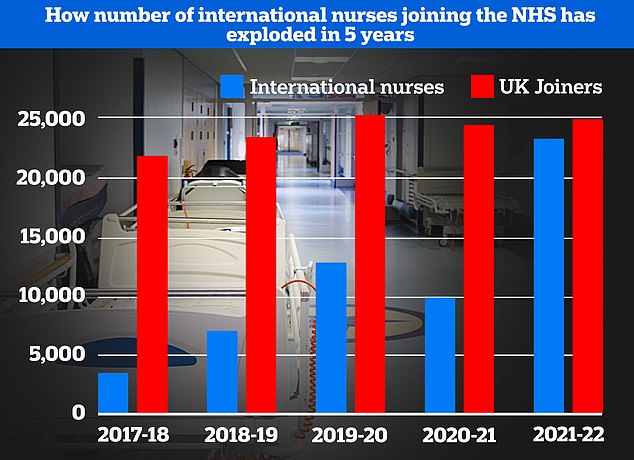
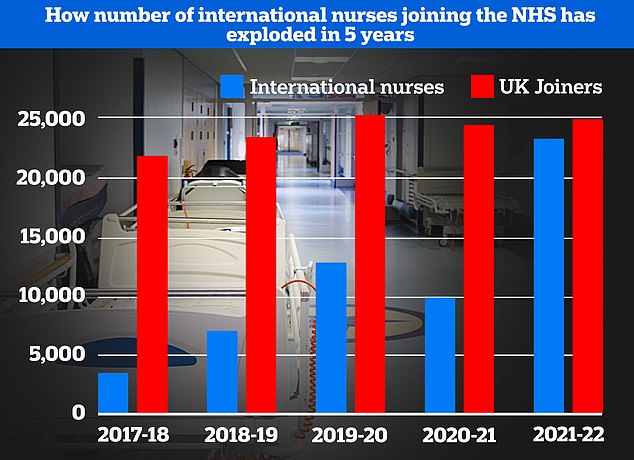
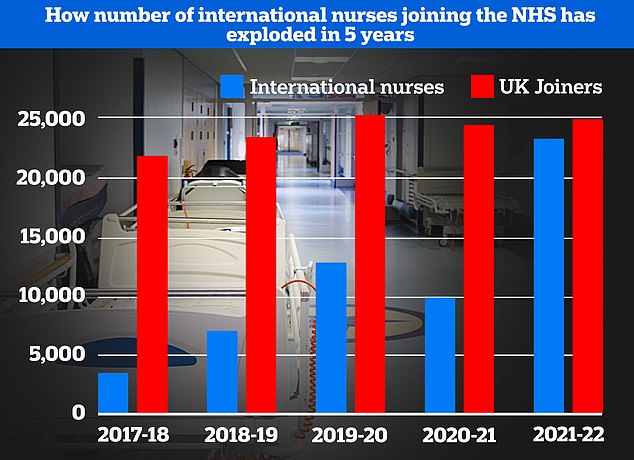
The number of internationally trained nurses joining the NHS has skyrocketed over recent years. Numbers have increased year-on-year, minus a blip of the Covid pandemic which hampered immigration, data from the Nursing and Midwifery Council shows. The number of international nurse recruits is now almost equal to the number of British nurses joining the profession for the first time
How is international recruitment affected?
The proposals will see the NHS ‘become less reliant on international recruitment’ in the ‘medium to long term’, the health service said.
Currently international staff make up almost a quarter (24 per cent) of all new joiners to the NHS annually.
By 2036/37 it is hoped this will fall to between nine and 10.5 per cent a year, the document said.
‘The NHS will always retain some level of overseas recruitment to give providers flexibility and as a source of wider and diverse talent,’ NHS England wrote.
The recruitment drive will also allow it to become less dependent on agency staff, cutting the bill for taxpayers by around £10billion between 2030 and 2037.
What are they planning with tech?
The plan has also pledged to invest in new technology.
This includes AI and robotics to cut admin time and ‘free up staff to focus on using their expertise to help patients’.
This includes speech recognition to aid with transcriptions to reduce clinic letter turnaround times and robotic assisted surgery.
Robotic process automation to carry out office tasks could also save close to 22million hours – equivalent to 2.9 million working days – over the next 10 years.
An expert group will be set to ‘identify advanced technology that can be used most effectively in the NHS’, the plan said.
Hub-and-spoke dispensing in pharmacies will also relieve some pressure on the community pharmacy workforce, the health service suggested.
This sees the hub prepare or assemble the medicines and send them back to the spoke pharmacy, which supplies the medicines to the patient.
Source: | This article originally belongs to Dailymail.co.uk