
Researchers have discovered that the experimental drug saracatinib, previously tested for potential use in treating various diseases, can significantly reduce inflammation related to atherosclerosis—a condition leading to heart disease. While saracatinib has shown promise in reducing plaque-based inflammation and shrinking plaque deposits in animal models, the team emphasizes the need for clinical trials to ensure its effectiveness in patients.
Potential new therapy emerges from”reverse-engineering” an existing compound.
A new study conducted by researchers at NYU Grossman School of Medicine suggests that an experimental drug, previously tested for the potential treatment of cancer, lung, and Alzheimer’s disease, could help slow down the progression of atherosclerosis that leads to heart disease.
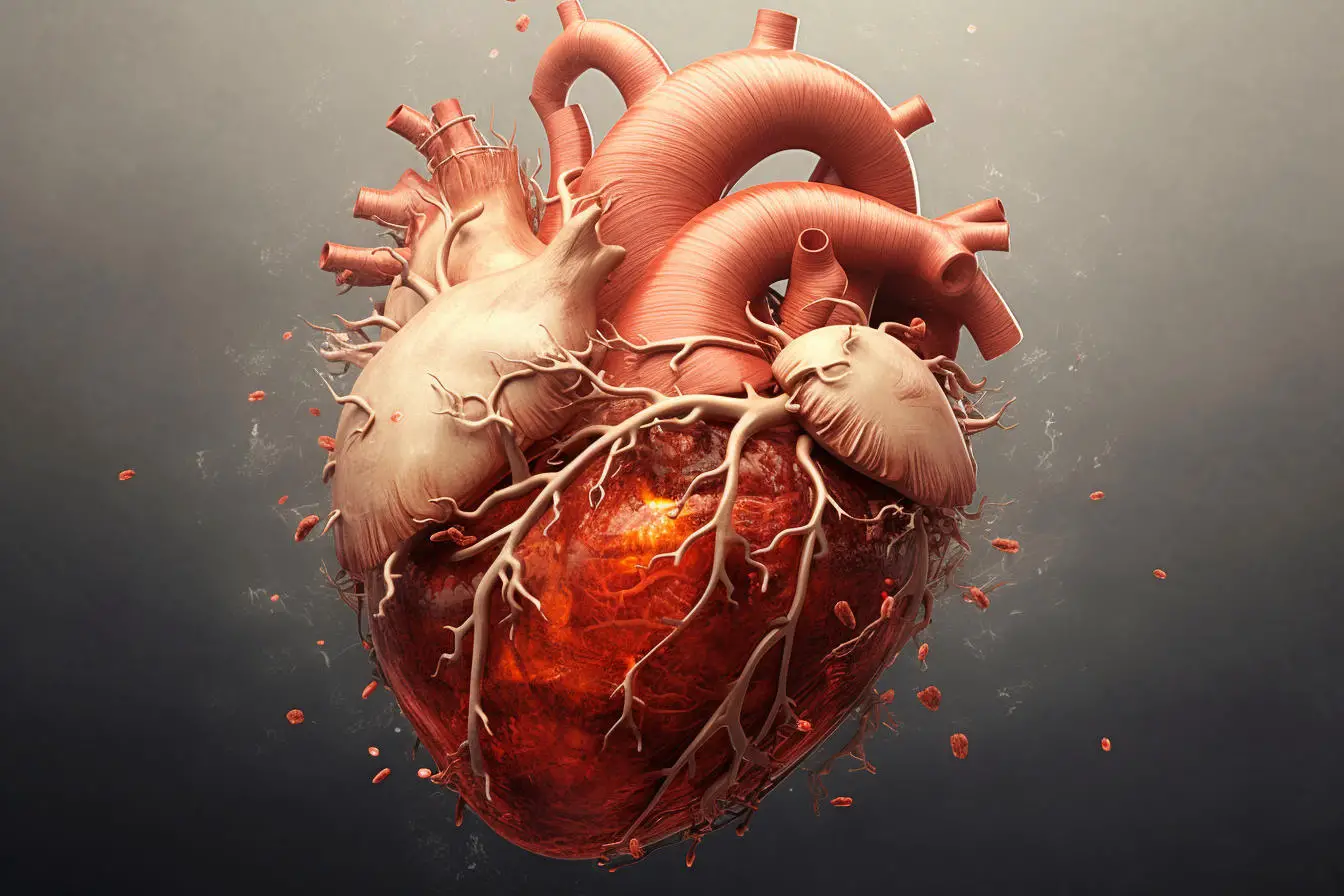
The study examines the underlying mechanisms of atherosclerosis, a condition characterized by the accumulation of fatty deposits within blood vessels. This accumulation can harden into plaques, triggering misplaced immune reactions (inflammation). Such a scenario can obstruct blood flow, leading to serious cardiovascular events like heart attacks or strokes.
Publishing June 8 in the journal Nature Cardiovascular Research, the new study showed that plasma (the liquid part of blood) from patients with atherosclerotic disease triggers an usually high inflammatory signal in blood immune cells. Further experiments then showed that the drug saracatinib reduced this inflammation signaling by more than 90% in human blood samples and diseased tissue samples.
“Our findings provide new insight into the inflammatory mechanisms in atherosclerosis and suggest for the first time that saracatinib may offer an effective therapy in cases where standard therapy, in the form of statins, fails to help,” says study co-lead author Letizia Amadori, PhD, a senior research scientist at NYU Langone Health.
Physicians prescribe statins to reduce harmful fats in the blood, but studies show that even with reduced plaque deposits, inflammation persists in many patients, who remain at high risk for heart attack. According to the study authors, the causes of this chronic immune response in patients are not fully understood, and anti-inflammatory treatments are sometimes ineffective in patient studies.
For the study, the team analyzed blood samples from 34 men and women with the condition specifically termed atherosclerotic cardiovascular disease (ASCVD), all of whom were on statins, and compared them with samples from 24 healthy donors.
To home in on saracatinib, the study authors explored 4,823 genes including 277 already known to play a role in inflammation and produce cytokines and other proteins that promote a chronic immune response.
According to Amadori, the team reasoned that if a particular medication could stop all these molecules from being made, then it could calm the response.
Rather than trying to create a suitable drug from scratch, the researchers instead turned to a list of pharmaceuticals already approved or being tested for other uses. Specifically, they searched a series of datasets from the National Institutes of Health called the Library of Integrated Network-Based Cellular Signatures, which contains hundreds of thousands of test results mapping the effects of various molecules, signaling proteins, and genetic changes on human cells.
Because saracatinib was shown in this search to reverse the expression of target genes, the process by which genes are turned on to make proteins, the authors tested it in human cells, diseased tissue, and animal models to see if it could actually stop, slow, or reverse inflammation prompted by ASCVD.
Among the findings, the results revealed that saracatinib blocks gene activity responsible for producing inflammatory proteins such as interleukin-1 beta and interluekin-6 that maintain ASCVD’s immune reactivity. Notably, an inhibitor of interleukin-1 beta was shown to effectively prevent heart attack in an earlier trial. At the same time, the drug boosted genes known to make proteins that help clean up plaque deposits by transporting fat away from the arteries.
Further experiments in rabbits revealed that saracatinib reduced plaque-based inflammation by about 97% compared with untreated animals. Meanwhile in mice, the same therapy prompted up to an 80% reduction in cells linked to inflammation in plaques and shrunk plaque deposits between 48% and 70%, depending on the dose of the medication, says Amadori.
“Our reverse-engineering method of finding new uses for old drugs can, in theory, be harnessed to uncover therapies for practically any disease that involves inflammation,” said study senior author Chiara Giannarelli, MD, Ph.D. “Since these chemicals have already been tested for safety, this technique offers a swift and cost-effective approach to pharmaceutical development.”
Giannarelli, an associate professor in the Departments of Medicine and Pathology at NYU Langone, says the study team next plans to use their same protocol to explore potential treatments for other inflammatory conditions linked to ASCVD, such as rheumatic arthritis or type 2 diabetes.
That said, Giannarelli cautions that while saracatinib appears promising, it must still be clinically tested to ensure that the treatment actually works in patients.
Reference: “Systems immunology-based drug repurposing framework to target inflammation in atherosclerosis” by Letizia Amadori, Claudia Calcagno, Dawn M. Fernandez, Simon Koplev, Nicolas Fernandez, Ravneet Kaur, Pauline Mury, Nayaab S Khan, Swathy Sajja, Roza Shamailova, Yannick Cyr, Minji Jeon, Christopher A. Hill, Peik Sean Chong, Sonum Naidu, Ken Sakurai, Adam Ali Ghotbi, Raphael Soler, Natalia Eberhardt, Adeeb Rahman, Peter Faries, Kathryn J. Moore, Zahi A. Fayad, Avi Ma’ayan and Chiara Giannarelli, 8 June 2023, Nature Cardiovascular Research.
DOI: 10.1038/s44161-023-00278-y
Funding for the study was provided by National Institutes of Health (NIH) grants.
Giannarelli is an inventor of a patent pending for this therapeutic approach to treat ASCVD as well as for the team’s drug development pathway. The terms and conditions are being managed in accordance with the policies and practices of the Icahn School of Medicine at Mount Sinai and NYU Langone Health.