The Dose21:13What should I know about group A strep?
Group A streptococcus has been in the headlines recently after 15 kids died in the U.K. Dr. Joanne Langley, a pediatrician specializing in infectious diseases, discussed what guardians and adults should know about this bacteria that can cause a range of illnesses.
- Several European countries are seeing a rise in scarlet fever, invasive group A streptococcus (iGAS).
- 2 Montreal children have died as a result of complications from iGAS.
- Some Canadian doctors have noticed an increase in iGAS infections.
- Doctors recommend good hand hygiene, flu shots and keeping an eye out for specific symptoms.
Two children in Montreal have died of complications related to invasive group A streptococcus (iGAS) infections, and pediatric infectious disease doctors say parents should be aware of symptoms as outbreaks of scarlet fever and iGAS infections emerge in other countries.
“Even though [severe iGAS infections] may turn out to be more common as we move through this high incidence of flu and RSV, they will still be relatively rare. That being said, it’s good to be on the lookout,” Dr. Joanne Langley, a pediatrician specializing in infectious diseases, told Dr. Brian Goldman, host of CBC’s The Dose.
Montreal Public Health said Friday that two children, both under the age of two, had died as a result of complications related to invasive group A strep. In all, four children have come down with the infection since mid-November. Officials say that’s above average for this kind of infection.
“It’s unclear at this point what is causing the increase that we are seeing in Montreal, and the increase that we’re seeing in different countries around the world now,” said Dr. Geneviève Bergeron, Montreal’s medical officer responsible for health emergencies and infectious diseases.
“It could be related to increased transmission after the pandemic period where there is more mixing. It also could be related to the circulation of other viruses.”
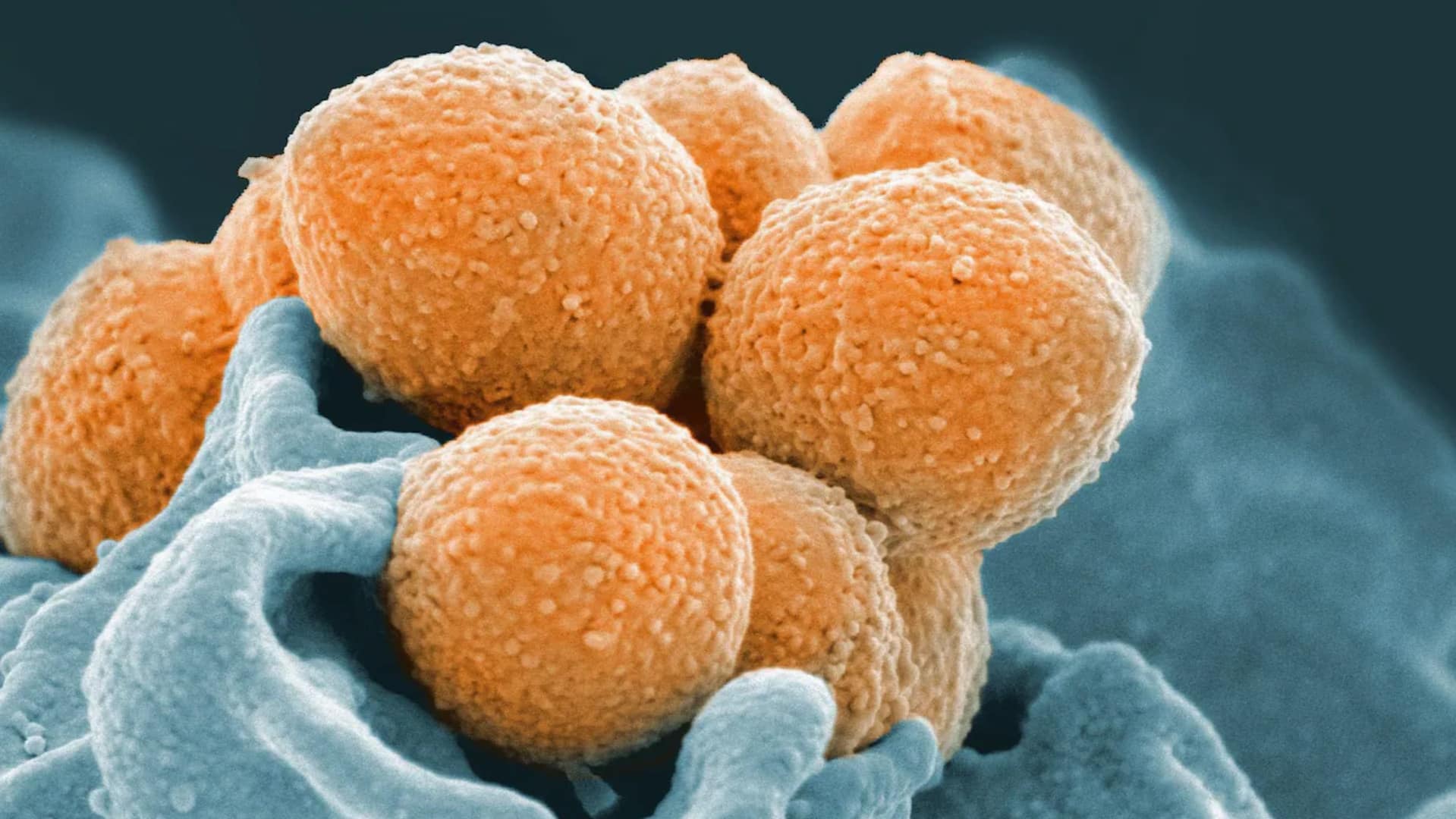
When group A strep becomes severe, it is known as invasive group A streptococcus, or iGAS. That happens when the bacteria get into parts of the body where bacteria don’t normally exist — like blood, the brain and the lungs.
Montreal Public Health said it encourages clinicians to promptly offer the appropriate care, including prescribing antibiotics.
At least 16 children in the U.K. have died in the last few months from conditions related to iGAS. The World Health Organization (WHO) says children under 10 are the most affected age group.
The Centers for Disease Control in the U.S. is also investigating a possible rise in invasive group A strep infections among kids. WHO and the European Centre for Disease Control & Prevention (ECDC) also urged caution this week about these infections in Europe.
Some pediatric infectious disease physicians say that anecdotally, they’ve recently noticed more iGAS infections.
“In my work these last two weeks on the wards, we have lots of invasive group A strep. We’ve got children across our hospitals going to the ICU for invasive group A strep,” Dr. Fatima Kakkar, a pediatrician and infectious disease specialist at Ste-Justine Hospital in Montreal, told CBC’s World This Weekend.
At this time, the U.K. cluster “does not pose an increasing risk” of iGAS disease in Canada, a Public Health Agency of Canada (PHAC) spokesperson said in a statement sent via email on Tuesday.
Dr. Jim Kellner, pediatric infectious disease physician at Alberta Children’s Hospital, says people should be aware of the broad range of illnesses that can be caused by this bacteria.
“On the one hand, it’s a minor pathogen that causes milder disease and at the other end of the spectrum can cause life-threatening disease,” said Kellner, who is also a professor of pediatrics at the University of Calgary.
Here’s what doctors say you should know about group A strep.
What is group A strep?
Group A streptococcus (GAS) are bacteria that live in the throat and the skin.
There are more than a hundred different strains of GAS, which is typically harmless for most people.
At least nine children have died in a recent outbreak of streptococcus A, and there are concerns over whether there’s enough penicillin in the country to treat the bacterial infections.
“You could be colonized with group A strep and it can just be there harmlessly, not bothering you,” said Dr. David Fisman, a professor of epidemiology at the University of Toronto’s Dalla Lana School of Public Health.
“Or, especially in kids and in other age groups, it can cause an infection in the back of your throat, which we commonly referred to as strep throat,” he told CBC’s Day 6.
Two of the more serious illnesses caused by iGAS infections are streptococcal toxic shock syndrome (STSS) and necrotizing fasciitis, or flesh-eating disease.
Other illnesses include meningitis and septic arthritis.
Langley and Kellner emphasize that these more serious illnesses are rare.
Is it circulating in Canada right now?
Montreal Public Health said it knows of four confirmed cases of iGAS since mid-November. Anecdotally, some doctors elsewhere in Canada have noticed more iGAS infections here.
According to Langley, who is also a researcher at Dalhousie University’s Canadian Center for Vaccinology, that may be happening because we know that iGAS infections can happen “after certain viral illnesses, particularly after influenza and after chickenpox.”
With several other viral illnesses circulating right now, that may be why some doctors are seeing more iGAS infections, says Dr. Jesse Papenburg, a pediatric infectious diseases physician at the Montreal Children’s Hospital.
“The viral infection kind of changes our natural immunity to the bacteria we have on us at all times,” he says.
“It’s been shown for different combinations of viruses and bacteria that yes, a viral illness can then put you at risk for a more severe bacterial infection.”
The World this Weekend23:53The World This Weekend Capsule Edition
On this episode, we speak with Dr. Fatima Kakkar about the Strep A outbreak in the U.K. Deana Sumanac-Johnson shows us how tutoring is helping students catch up from pandemic disruptions – but low resources are keeping it out of reach for many families. Plus, we take you to Prince George, B.C. – where volunteers are helping Ukrainians fleeing the war adjust to life in Canada.
Group A strep circulates in Canada every year. PHAC spokesperson Anne Génier said in an email that iGAS is “endemic in Canada,” averaging anywhere from 2,000 to 3,000 cases annually.
In Canada, iGAS disease is nationally reported, but mild cases of GAS are not, according to PHAC.
Langley emphasizes that Canada is currently not seeing the same number of severe iGAS infections as other countries.
“To my knowledge, we are not seeing this phenomenon yet in Canada, but it would be picked up by our current surveillance system,” she said.
Who is most at risk for iGAS?
According to Langley, those most at risk are children under the age of one; those who haven’t been vaccinated against the flu or chickenpox; immunocompromised people and those with skin conditions that can allow bacteria to enter the body, such as uncontrolled eczema.
A chickenpox infection is also a risk factor.
“After chickenpox, your risk of an invasive group A strep infection is about 10 times elevated,” Langley said.
What are symptoms to watch out for in kids?
She says it’s very difficult for parents to recognize group A strep based on medical history and a physical alone.
“They really need to come for medical attention,” she said, noting a lab test would confirm group A strep.
Strep throat is the most common infection in kids, Kellner says. The treatment is typically a penicillin-type antibiotic.
Langley says another common infection from group A strep is the skin infection impetigo.
For those wondering which symptoms may indicate a severe iGAS infection, Langley says guardians should watch for any symptoms worse than “a regular runny nose or a cough.”
Specifically, she listed the following red-flag symptoms in children that mean parents should seek medical attention immediately:
- Trouble breathing
- Fever
- Significant change in personality
- Fatigue
- Stiff neck
- A full-body rash
- Not able to eat or drink
- No longer urinating
Kakkar says that if a child has recently had a viral illness like the flu, parents should watch for more severe symptoms for up to a week after flu symptoms began.
She also highly recommends children get their flu shots.
“Most severe cases of group A strep are happening after influenza. So if parents can get their children vaccinated, this will definitely help reduce the risk of having this serious secondary complication.”
What do symptoms look like in adults?
Signs of a possible serious infection in adults are high fever, difficulty breathing, fatigue and confusion.
Widespread reddening of the skin is also another symptom, Langley says.
How can people protect themselves and children?
Other than looking for signs of illness and changes to well-being, Langley recommends proper hand washing before eating and after coughing or sneezing, and watching for skin infections.
PHAC officials also recommend people cough or sneeze into a tissue or into their bent elbow, and disinfect frequently touched surfaces and objects.
Langley recommends visiting or speaking with a health-care provider if a child does have a suspected strep throat infection.
“Group A strep sore throat may be fairly common, but it is very unlikely to go on to an invasive group A strep infection,” she said.