
Chris Toner, an emergency nurse at Northern Ireland’s biggest hospital, loves his vocation. But as NHS staff strike for better pay and conditions this week, he admits that he often hates his job.
“It never lets up. You’re burned out constantly. You hate having to come into work in the mornings,” said Toner at Belfast’s Royal Victoria Hospital (RVH), where the pressures that have led to NHS strike action being called in England, Wales and Northern Ireland from Monday are among the most acute in the UK.
In Northern Ireland, the national health service is critically ill. The region spends nearly half of its total budget on healthcare but its waiting lists are by far the longest in the UK.
Pay for the region’s nurses has not kept pace with the rest of the UK. In 2019 they held their first strike in a century to achieve parity.
Their wages slipped behind again this year because there was no regional assembly to sign off a 4.5 per cent pay rise because of a political row over post-Brexit trading arrangements that has paralysed the region’s executive since May. Officials only approved the increase on December 8.
Ray Rafferty, trades union chair for the Belfast trust which covers 13 health service unions, said it was “too little, too late”.
Even before the Covid-19 pandemic, the number of people waiting more than a year to see a consultant was 100 times higher than in England. Well over half a million people — 30 per cent of the population — are currently waiting for appointments, admission or diagnostic tests.
Meanwhile, the number of GPs has been falling for years, driving more people to clogged-up hospitals where patients face a median wait before admission of 13 hours and 19 minutes in A&E, according to official data.
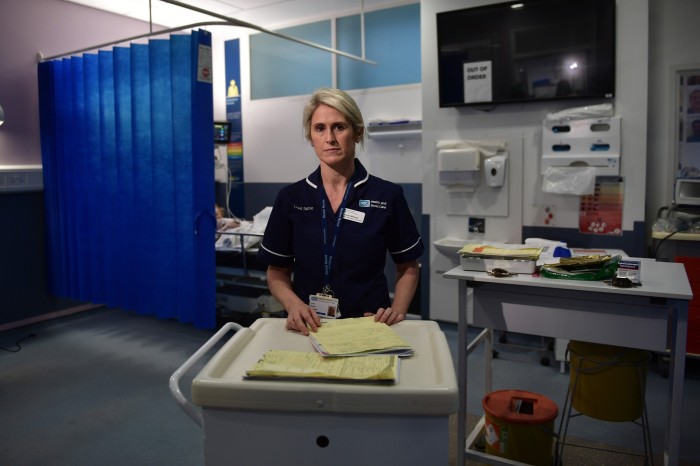
Claire Wilmont, 39, a lead nurse at the RVH, regularly starts her shift with 60 to 80 patients stuck on beds or chairs sandwiched into the emergency department without a place on a ward to go to. “What we are facing is severe, ongoing, huge numbers of patients,” she said. “In 18 years [in the emergency department], I’ve never seen it as bad as this.”
Toner, 31, does not want to quit but said he can understand those who do. “You can work in Starbucks and get paid the same,” he said. “With all the pressure [here], is it worth it?”
Gary Clarke, a paramedic with the Northern Ireland Ambulance Service, recalls staying with a patient outside a hospital for 9½ hours this summer; the patient had been waiting with another crew for seven hours before that.
“I’m not a big fan of strikes but I think in this current climate . . . after years of underpayment . . . if it’s not [a rise of] 5 to 8 per cent, don’t even bother.”

But pay is not the only problem: nurses say overcrowding compromises patient safety. Seven reports into Northern Ireland’s health service in the past 20 years have identified ways to improve the system.
One solution is to set up regional centres of excellence — but shutting any hospital, even to deliver care more efficiently elsewhere, is fraught.
“Politicians are unlikely to close a hospital . . . for fear of losing crucial votes,” wrote Ciaran O’Neill, an expert on public health at Queen’s University in Belfast, and Dame Carol Propper, an economics professor at Imperial College in London, in a recent study.
NHS hospital care costs in Northern Ireland have risen about 28 per cent since 2016, over three times the rate in England.

More than a third of those waiting for an outpatient appointment with a consultant have been waiting at least two years. By March 2023, the goal is for 50 per cent to get an appointment within nine weeks and no one to be waiting more than a year but these targets look unattainable.
Brian Armstrong, director of unscheduled care at the RVH — who supports staff’s right to strike, despite being a senior NHS manager — acknowledged that the action “will further impact waiting lists, of course it will”.
With weeks of strikes looming across the UK in a range of sectors he said: “I worry [the government] will feel obliged to hold the line. The NHS is vulnerable. We can’t allow strikes to go on too long.”
Private healthcare could offer a “safety valve to tackle these [waiting lists],” according to Mark Regan, chief executive of Kingsbridge Private Hospital in Belfast. But he added: “I’ve always been in favour of healthcare that’s free at the point of delivery. You can opt out if you want to go private, but you shouldn’t have to go private.”
Regan said the number of surgeries performed by Kingsbridge, the region’s biggest private hospital group, had almost tripled in the past decade, and not just for the wealthy. The second-largest number of patients came from West Belfast, one of Northern Ireland’s most socially and economically deprived areas.
Because of the pressures NHS nurses may be attracted to the private sector by safer staff-to-patient ratios and a sense they are valued; other health professionals are looking to go abroad.

Mark O’Hare, a school vice-principal, said his brother, a consultant in accident and emergency, had moved to Perth, Australia and “he’s earning twice the money for half the work”.
While he supports the NHS, which he thanks for performing a double lung transplant on his wife, he has taken out private health insurance himself for £20 per month to have the security of being able to see a consultant within two weeks.
“It’s the waiting lists,” he said. “If you need it, it’ll be the cheapest £20 a month you’ve ever spent.”