
Jeannette Rogers believes if there was a sobering centre in Halifax, her son may have never died in a police jail cell.
Halifax regional council will vote Tuesday on a proposed sobering centre — a short-term recovery facility staffed mainly by peer support workers — and one that Jeanette Rogers says her son, Corey Rogers, would have benefited from on the night of June 15, 2016.
“Over the long term, I think he might have gotten the help that he needed,” said Rogers. “And he would’ve survived.”
Corey Rogers was arrested for public intoxication in June 2016 outside the hospital where his wife had given birth to their baby.
Police officers said the 41-year old spat at them so they put a spit hood over his head and carried him into a jail cell. He suffocated and died less than an hour later.
Rogers had a “lengthy record” of being arrested and put in a cell for public intoxication, according to court documents.
His mother believes if he was taken to a facility where he wasn’t treated like a criminal he may still be here today.
A proposed three-year pilot project before Halifax regional council would see the municipality partner with the province to create a sobering centre. The motion comes after two years of research and consultation by Halifax’s Public Safety Office.
It recommends establishing a facility with the capacity to care for at least 10 people. Halifax and the province would split costs of approximately $278,000 this year and $980,000 each of the next two years.
Staffing would include peer support workers and culturally appropriate and gender inclusive supports but there’s no mention of medical health professionals in the motion.
The goal, it says, would be to connect patients with the proper services, reduce pressure on first responders and hospital emergency rooms and stop criminalizing addiction.
“It really provides the right service, in the right place, by the right people, at the right time,” said Dr. Leah Genge, a family physician who specializes in addiction medicine.
Genge works with the Mobile Outreach Street Health program in Halifax. She says she has seen the negative effects of criminalizing addiction.
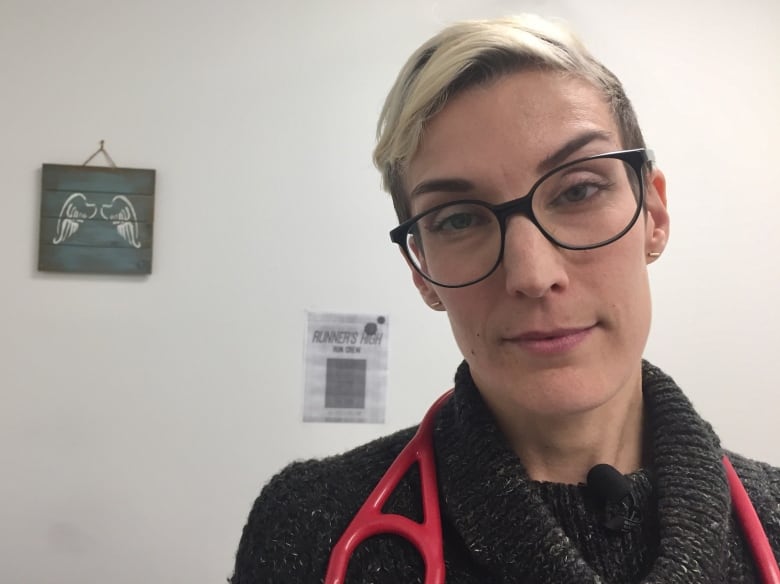
“I see a lot of people who are suffering. Who have had unimaginably difficult lives and continue to have unimaginably difficult lives,” she said. “It all comes down to humanity.”
A lot of the work the outreach program does is building trust with people who are hesitant to use the heath care system, she said.
Genge also worked with the Alpha House in Calgary, a sobering centre that offers additional services aimed at homelessness, addiction and mental health treatment and resources for people to stay longer if needed.
“It was a safe place that people always knew they could go to, right? If they couldn’t go anywhere else, they could go there,” she said.
Genge says Nova Scotia’s current response to addiction is not good enough.
“I think we have a lot of work to do in the province,” Genge said. “We have a lot of work to do in every aspect of addiction care.”
The province’s chief officer of mental health and addictions agrees.
“We have a long way to go, I think, to get to a place where we have everything that addiction medicine providers would like to see,” Dr. Sam Hickcox said. “But we have come so far.”
Hickcox says he’s seen significant progress during the 10 years he’s practised addiction medicine.
There are more doctors working in addiction, it’s easier to access medication like methadone and there are new initiatives like the Overlook harm-reduction housing project and the addiction and mental health recovering centres, he said.
Hickcox says a sobering centre is a good example of harm reduction that has been successful in other jurisdictions and could work in Halifax.
“First and foremost, staff need to have empathy and compassion,” he said. Once trust is established, he said, the facility can be used as an entry point for other types of care and support.
Public intoxication arrests
Hundreds of people are put in a jail cell for public intoxication every year in Halifax, according to Halifax Regional Police.
There were more than 1,700 intakes in 2018 and nearly 1,600 in 2019. That number dropped to 528 in 2020.
Halifax Regional Police denied an interview request, but in a statement a spokesperson said the department supports harm reduction and would work with community stakeholders to develop such initiatives.
The officers and cell guards who arrested Corey Rogers and put him in a cell did not follow policy.
They left Rogers lying on the ground with a spit hood on his head and didn’t check on him for several hours until they found him dead. Police place spit hoods over the heads of prisoners to prevent being bitten or spat upon. Their use has been criticized particularly if prisoners vomit inside the hood, creating a choking risk.
There has to be a better alternative than an empty concrete room, Jeannette Rogers says.
“We learned six years ago that’s not always a good place for someone who’s intoxicated.”