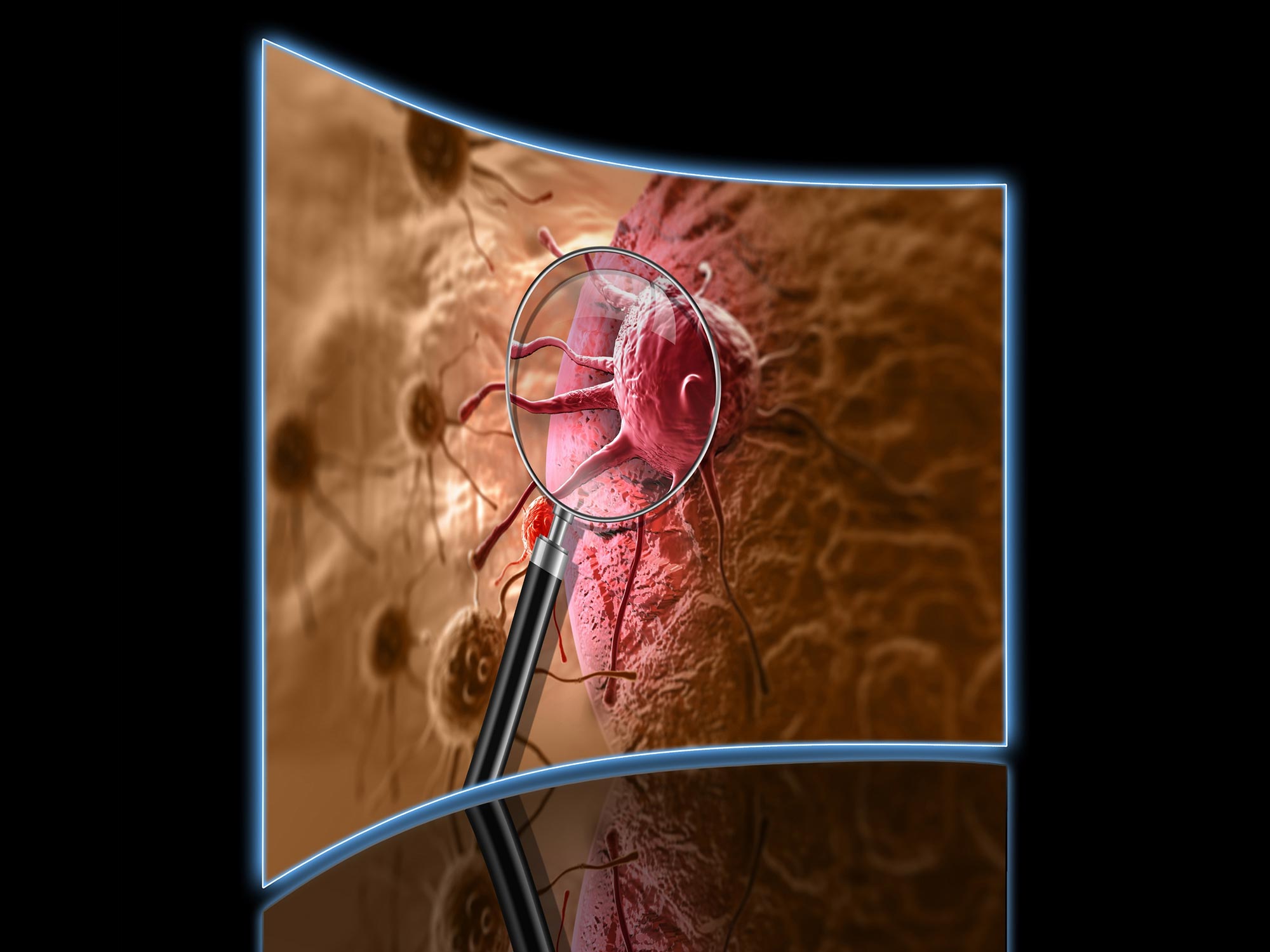
Gliomas are a type of tumor that occurs in both the brain and spinal cord.
The study provides key information about gliomas’ size and growth rate.
An important new hint for preventing and treating brain tumors known as gliomas has been discovered in research headed by the Lunenfeld-Tannenbaum Research Institute (LTRI) at Mount Sinai Hospital in Toronto, as well as the Mayo Clinic Comprehensive Cancer Center and the Mayo Clinic Center for Individualized Medicine. The discovery, which was published in the journal Science, offers a unique glimpse into the biological changes driving the growth of gliomas.
Researchers discovered that, when compared to animal models lacking the alteration, animals with the germline alteration rs55705857 developed gliomas significantly more frequently and in half the time. The results are also relevant to other cancers and disorders in addition to brain tumors.
“While we understand much of the biologic function of germline alterations within genes that code for proteins, we know very little about the biologic function of germline alterations outside of genes that code for proteins. In some way, these germline alterations interact with other mutations in cells to accelerate tumor formation,” says co-lead author Robert Jenkins, M.D., Ph.D., a genetics researcher at Mayo Clinic in Rochester. “Based on this new understanding of its mechanism of action, future research may lead to novel and specific therapies that target the rs55705857 alteration.”
The study offers new knowledge that may help clinicians determine, pre-surgery, whether a patient has a glioma.
“We expected that rs55705857 would accelerate low-grade glioma development, but we were surprised by the magnitude of that acceleration,” says co-lead author Daniel Schramek, Ph.D., a researcher at Lunenfeld-Tannenbaum Research Institute.
There are many alterations, likely thousands, outside of genes associated with the development of cancer and other diseases, but the mechanism of action is only understood for very few, Dr. Schramek says.
This study demonstrates that, with the tools of modern molecular/cell biology, it is possible to decipher much of the mechanism of action of such alterations.
Reference: “A noncoding single-nucleotide polymorphism at 8q24 drives IDH1-mutant glioma formation” by Connor Yanchus, Kristen L. Drucker, Thomas M. Kollmeyer, Ricky Tsai, Warren Winick-Ng, Minggao Liang, Ahmad Malik, Judy Pawling, Silvana B. De Lorenzo, Asma Ali, Paul A. Decker, Matt L. Kosel, Arijit Panda, Khalid N. Al-Zahrani, Lingyan Jiang, Jared W. L. Browning, Chris Lowden, Michael Geuenich, J. Javier Hernandez, Jessica T. Gosio, Musaddeque Ahmed, Sampath Kumar Loganathan, Jacob Berman, Daniel Trcka, Kulandaimanuvel Antony Michealraj, Jerome Fortin, Brittany Carson, Ethan W. Hollingsworth, Sandra Jacinto, Parisa Mazrooei, Lily Zhou, Andrew Elia, Mathieu Lupien, Housheng Hansen He, Daniel J. Murphy, Liguo Wang, Alexej Abyzov, James W. Dennis, Philipp G. Maass, Kieran Campbell, Michael D. Wilson, Daniel H. Lachance, Margaret Wrensch, John Wiencke, Tak Mak, Len A. Pennacchio, Diane E. Dickel, Axel Visel, Jeffrey Wrana, Michael D. Taylor, Gelareh Zadeh, Peter Dirks, Jeanette E. Eckel-Passow, Liliana Attisano, Ana Pombo, Cristiane M. Ida, Evgeny Z. Kvon, Robert B. Jenkins and Daniel Schramek, 6 October 2022, Science.
DOI: 10.1126/science.abj2890