
A new gene therapy that inhibits targeted nerve cell signaling effectively reduced neuropathic pain in mice with spinal cord or peripheral nerve injuries with no detectable side effects.
In mouse studies, pain-blocking neurotransmitters produced long-lasting benefits without detectable side effects.
An international team of researchers led by scientists at the University of California San Diego School of Medicine reported that a gene therapy that inhibits targeted nerve cell signaling effectively reduced neuropathic pain in mice with spinal cord or peripheral nerve injuries with no detectable side effects.
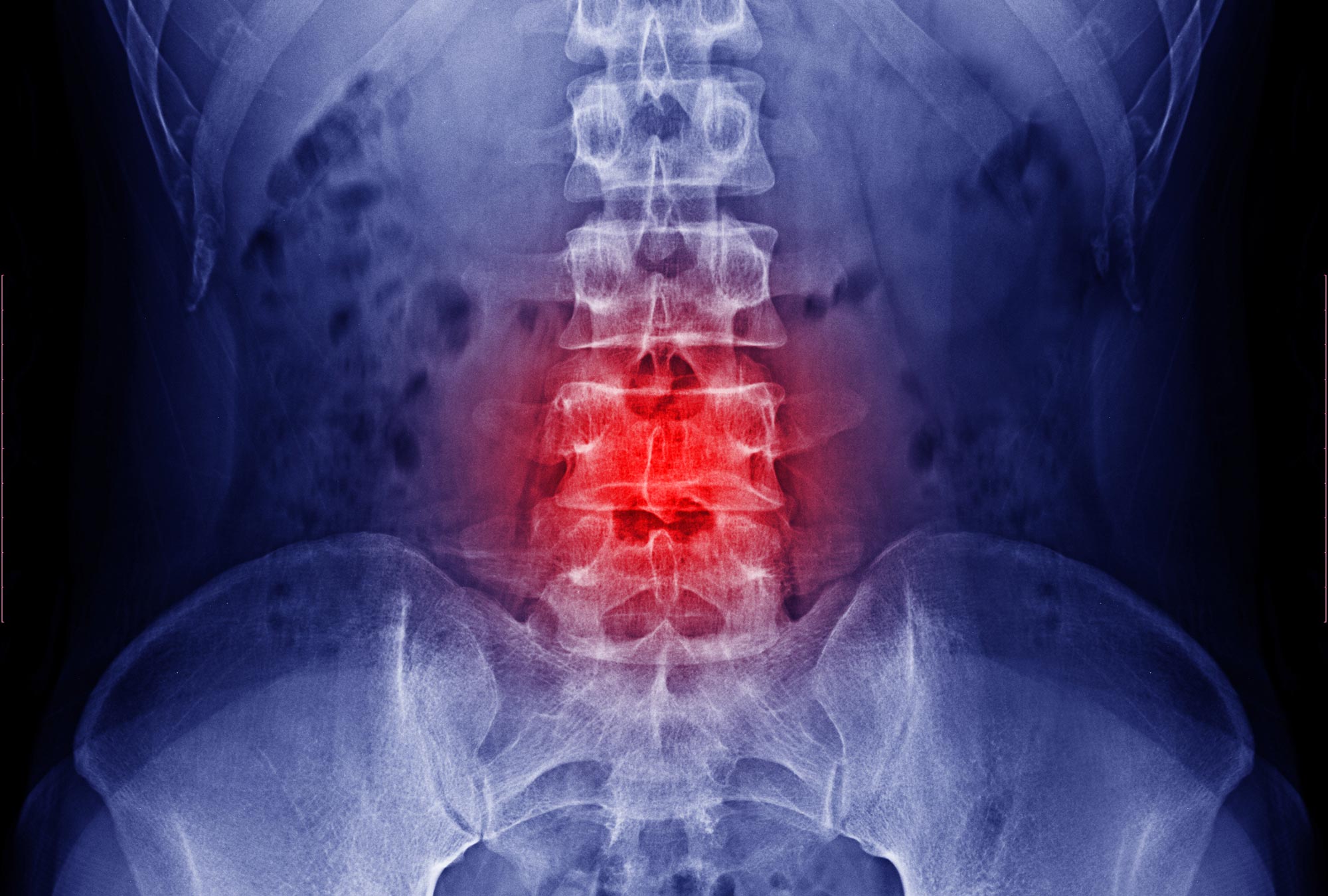
The results, which were published in the online edition of Molecular Therapy on May 5, 2022, suggest a possible new treatment option for a condition that may affect more than half of individuals with spinal cord injuries. Neuropathy involves damage or dysfunction in nerves elsewhere in the body, typically resulting in chronic or debilitating numbness, tingling, muscle weakness, and pain.
There are no singularly effective remedies for neuropathy. Pharmaceutical therapy, for example, may need sophisticated, continuous medication administration and is linked with adverse side effects such as drowsiness and motor weakness. Opioids may be effective, but they can also develop tolerance and raise the risk of overuse or addiction.
Because physicians and researchers are able to pinpoint the precise location of a spinal cord injury and the origin of neuropathic pain, there has been much effort to develop treatments that selectively target impaired or damaged neurons in the affected spinal segments.
In recent years, gene therapy has proven an increasingly attractive possibility. In the latest study, researchers injected a harmless adeno-associated virus carrying a pair of transgenes that encode for gamma-aminobutyric acid or GABA into mice with sciatic nerve injuries and consequential neuropathic pain. GABA is a neurotransmitter that blocks impulses between nerve cells; in this case, pain signals.
The delivery and expression of the transgenes — GAD65 and VGAT — were restricted to the area of sciatic nerve injury in the mice and, as a result, there were no detectable side effects, such as motor weakness or loss of normal sensation. The production of GABA by the transgenes resulted in measurable inhibition of pain-signaling neurons in the mice, which persisted for at least 2.5 months after treatment.

Senior study author Martin Marsala, MD, is a professor in the Department of Anesthesiology at UC San Diego School of Medicine. Credit: UC San Diego Health Sciences
“One of the prerequisites of a clinically acceptable antinociceptive (pain-blocking) therapy is minimal or no side effects like muscle weakness, general sedation or development of tolerance for the treatment,” said senior author Martin Marsala, MD, professor in the Department of Anesthesiology in the UC San Diego School of Medicine.
“A single treatment invention that provides long-lasting therapeutic effect is also highly desirable. These findings suggest a path forward on both.”
Reference: “Precision spinal gene delivery-induced functional switch in nociceptive neurons reverses neuropathic pain” by Takahiro Tadokoro, Mariana Bravo-Hernandez, Kirill Agashkov, Yoshiomi Kobayashi, Oleksandr Platoshyn, Michael Navarro, Silvia Marsala, Atsushi Miyanohara, Tetsuya Yoshizumi, Michiko Shigyo, Volodymyr Krotov, Stefan Juhas, Jana Juhasova, Duong Nguyen, Helena Kupcova Skalnikova, Jan Motlik, Hana Studenovska, Vladimir Proks, Rajiv Reddy, Shawn P. Driscoll, Thomas D. Glenn, Taratorn Kemthong, Suchinda Malaivijitnond, Zoltan Tomori, Ivo Vanicky, Manabu Kakinohana, Samuel L. Pfaff, Joseph Ciacci, Pavel Belan and Martin Marsala, 5 May 2022, Molecular Therapy.
DOI: 10.1016/j.ymthe.2022.04.023